Servicemembers, Veterans Take Their Own Lives at Higher Rates
WASHINGTON—In recent decades, suicide rates have soared in the United States, increasing 25% from 1999 to 2016.
The issue has been especially acute among military servicemembers and veterans. During the same time period, the DoD’s active component suicide rate leapt from 10.7 to 21.5 suicide-related deaths per 100,000 servicemembers. Veterans, meanwhile, have a 21% higher suicide rate than age- and sex-matched civilian cohorts, resulting in a shocking average of 20 veterans taking their lives each day.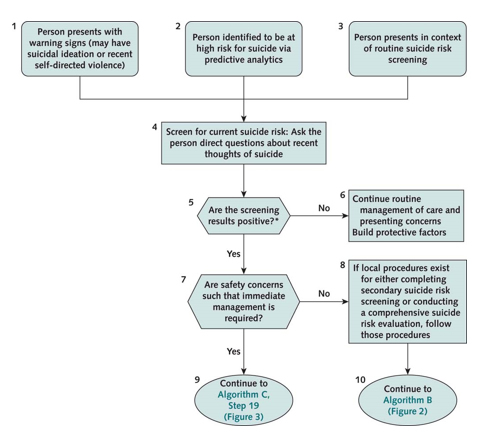
In an effort to curb the suicide epidemic, the VA and DoD approved this spring an update to the 2013 joint clinical practice guideline for assessing and managing patients who are at risk for suicide.
The new guideline was designed to provide federal healthcare providers a framework by which to screen for, evaluate, treat and manage the individual needs and preferences of VA and DoD patients who might be at risk for suicide, according to a synopsis published in Annals of Internal Medicine.1
The process began in January 2018, when the VA/DoD Evidence-Based Practice Work Group convened to develop a joint VA/DoD guideline. The panel drafted key questions, systematically searched and evaluated the literature through April 2018, created algorithms, and advanced 22 recommendations in accordance with the Grading of Recommendations Assessment, Development and Evaluation system.
Recommendations include three clinical practice algorithms addressing screening and evaluation, risk management and treatment and other management methods. In addition, the guideline panel formulated 22 evidence-based recommendations organized into three categories.
Continue: Risk Factors
