Report Highlights Pitfalls of Outside Care for Veterans

Damage Controlman 3rd Class Sergio Viscarra and Damage Controlman 3rd Class Katelyn Bingaman, assigned to Arleigh Burke-class guided-missile destroyer, USS John S. McCain (DDG 56), speak to veterans at the Portland, OR, VAMC last month for the annual Rose Festival during Portland Fleet WeekU.S. Navy photo by Mass Communication Specialist Seaman Sophia H. Bumps
WASHINGTON — Patient satisfaction is higher with care received at VA hospitals than most community facilities, according to recent federal data which bolsters previous evidence of comparatively high-quality care provided by VHA facilities.
In fact, VA hospitals outperformed non-VA hospitals on all 10 core patient satisfaction metrics, including overall hospital rating, communication with doctors, communication about medication and the willingness to recommend the hospital, according to Medicare’s latest nationwide survey of patients.
Earlier this year, another review determined that care provided in the VA healthcare system is consistently as good as or better than non-VA care in terms of clinical quality and safety. The systematic review from the RAND Corp. compared care provided in VA and non-VA settings and included published studies from 2015 to 2023, updating two prior systematic reviews on this topic.1
Recently, an article published in a RAND publication looked at the challenges and benefits of increasing community care funded by the VA. It raised concerns about rising costs and poor coordination.2
Based on the recent survey, Medicare awarded star ratings from one star to five stars, with five representing the best quality care. Patient surveys received between July 2021 and June 2022 gave 72% of VA hospitals four or five stars for overall hospital rating compared to 48% of reporting non-VA hospitals.
Other areas in which VA hospitals received a higher percentage of four- or five-star ratings than non-VA hospitals on the Care Compare website were:
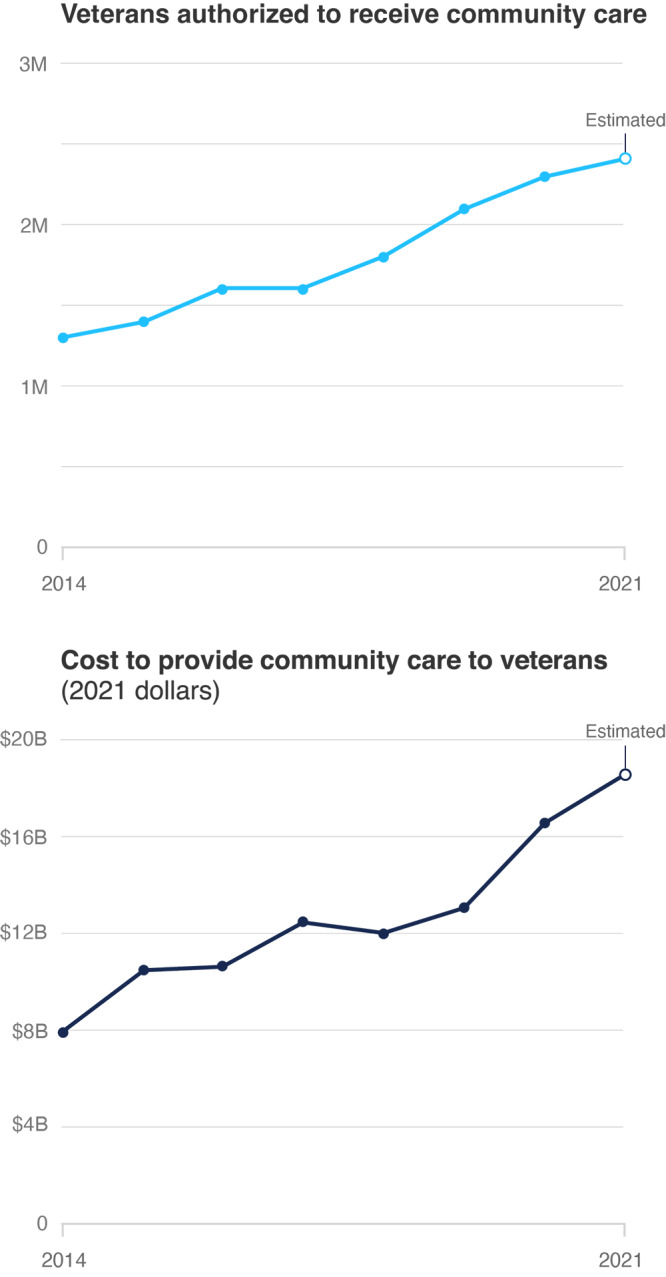
Click to Enlarge: Number of Veterans Eligible for VHA Funded Community Care Over Time and the Cost of Providing That Care.
Source: Congressional Budget Office, 2021, p. 7, Table 1. Estimated number of veterans authorized to receive community care in 2021 extrapolated from LaPuz, 2022. Estimated costs to provide community care in 2021 are from U.S. Department of Veterans Affairs, 2022b.
NOTE: The Congressional Budget Office’s definition of community care includes inpatient, outpatient, dental, mental health, prosthetics, and rehabilitation services from non-VHA providers, as well as long-term support, such as through nursing homes, noninstitutional care, and state facilities and programs. Those data do not reflect certain other services supported through community care funding, such as those for caregivers and Camp Lejeune Family Member Program participants.
Source: Rand Health Quarterly
- Communication with doctors (87% vs. 48%),
- Communication with nurses (59% vs. 35%),
- Responsiveness of hospital staff (63% vs. 34%),
- Communication about medicines (80% vs. 38%),
- Cleanliness of the hospital environment (69% vs. 52%),
- Quietness of the hospital environment (49% vs. 38%),
- Discharge information (65% vs. 55%),
- Care transition (76% vs. 35%), and
- Willingness to recommend the hospital (76% vs. 52%).
“At VA, veterans are the ultimate judges of our successes or failures—so we’re very proud to be this highly rated in a survey of veterans,” said VA Secretary Denis McDonough. “Our goal at VA is to deliver world-class care to every veteran, every time, and we will continue to invest in VA healthcare and the patient experience until we make that goal a reality.”
The Centers for Medicare and Medicaid Services update the Hospital Consumer Assessment of Healthcare Providers and Systems Star Ratings each quarter in a survey administered to a random sample of patients across the country.
Discharged patients are asked 29 questions about their recent hospital stay, including 19 core questions about critical aspects of patients’ hospital experiences. The HCAHPS survey is administered to a random sample of adult patients across medical conditions between 48 hours and six weeks after discharge; the survey is not restricted to Medicare beneficiaries.
The same questions are asked on VA and community hospital surveys to evaluate the patient experience.
VA also surveys veterans in order to understand and improve their healthcare experience. Based on 560,000 surveys, the VA Trust Report for the second quarter of fiscal year 2023 shows that nearly 90% of veterans who get their care from VA trust VA for their care. More than 79% of veterans trust VA overall, according to a press release, a 1.9% increase from the last quarter and a 24% increase since 2016.
Tracking both the quality of and patient satisfaction with VA healthcare is critical, according to the new report in Rand Health Quarterly because of growing concerns that increased use of community care by veterans might not be the panacea supporters had promoted.
“Since 2014, the number of veterans receiving community care has grown considerably, along with VA’s budget for community care,” RAND Corp. researchers wrote. “In July 2022 testimony to the House Veterans’ Affairs Committee, VA reported that community care accounted for 44% of its healthcare services across care settings. “
The report added that the total amount that VA has spent on community care has steadily increased, from $7.9 billion in 2014 to $18.5 billion in 2021. “As the costs for community care have risen, the share of the VHA budget that goes toward community care has also increased,” the authors noted. “In 2014, community care accounted for approximately 12% of VHA spending. However, this proportion had nearly doubled by 2021, with community care costs making up 20% of all VHA spending on medical care.”
VA’s fiscal year 2023 budget request suggested that community care would increase to 23% of the VHA medical care budget in 2023 and 25% in 2024
“Although comparisons between the cost of VHA-delivered and community care are limited, there are some indications that community care may be more expensive than VHA-delivered care,” according to the article. “VHA has the ability to manage and standardize the care that it delivers directly, but it is not able to manage veterans’ care once they have been referred to community providers. VHA officials have reported that local community care practice patterns, such as a greater use of X-rays and other imaging services, were a driver of higher-than-estimated spending on community care in 2017 and 2018. A recent analysis noted that VHA-delivered care costs less than comparable care from Medicare providers and produced better outcomes.”
RAND pointed out that tracking the quality of care provided through the Community Care Network “is necessary to identify whether and how the increased reliance on community care has affected veterans’ outcomes. Community care puts VHA into the role of a payer for health care as opposed to its traditional role as an integrated health system, in which it functions as both provider and payer. As a payer, VHA can hold third-party administrators responsible for implementing and managing the Community Care Network and accountable for the quality and adequacy of community care providers. To do this, VHA needs to set quality standards and performance metrics and either require providers to report on their ability to meet those expectations or conduct its own evaluations.”
In addition to cost, coordination with community care has presented problems for the VHA. “Poorly coordinated care between VHA and community care providers could result in confusion for patients, duplicative tests, increased costs, and lower-quality care,” according to the RAND article. “Research also suggests that the increased burden of coordinating care with non-VHA providers has resulted in higher rates of burnout among VHA primary care providers.”
In response, the VA created the Office of Integrated Veteran Care in October 2021, with a focus on improving coordination across care settings.
“Because this integrated care model is still being implemented and has not yet been established nationwide, it is not known whether and to what extent it will address care coordination challenges and improve care for veterans,” the authors noted.
Although long wait times were among the driving forces to increase access to community care, the report noted that mean wait times decreased between 2015 and 2018 for both VHA and community care, with the greatest declines at VHA facilities. By 2018, however, community care wait times were longer than VHA wait times, the researchers added.
On the other hand, the report said access appeared to have improved for some rural veterans.
Another issue has been a lack of understanding of veterans’ needs by community care providers, according to the RAND article, which explained, “VHA makes training available to community care providers to help increase their military/veteran cultural competency, familiarity with healthcare issues that are common among veterans, and aspects of specialized care. However, only a small proportion of community care providers have completed this training and VHA has no authority to require that they do so. Future evaluations of veterans’ care should explore links between community care providers’ familiarity with treating veterans and whether veteran patients’ full set of needs are being met, regardless of where they receive care.”
The authors called for future research on the benefits and challenges of community care, including:
- Modeling community care access and utilization. That would “help VHA better prepare for the volume of care that patients could require, improve the accuracy of budget estimates and allow for policy simulations to estimate the effect of potential policy changes, such as reforms to access standards.”
- Examine differences in health care quality and access between VHA-delivered and community care. “Policymakers must ensure that standards for community care are at least equal to those for VHA-delivered care. Veterans who see community care providers should be able to expect the same high quality of care that they receive from VHA providers.”
- Study differences in veterans’ experiences with community care. “It is essential that researchers examine potential disparities in care outcomes and experiences across veteran populations, such as by gender, race/ethnicity, sexual orientation and gender identity, geography, and VHA priority group.”
- Ask about community care providers’ experiences in delivering care to veterans. “Their perceptions of their readiness to treat veterans and the challenges they experience when working with VHA could also help inform policies and programs to improve care coordination and outreach efforts to increase community care providers’ familiarity with veterans and their needs.”
- O’Hanlon C, Huang C, Sloss E, Anhang Price R, Hussey P, Farmer C, Gidengil C. Comparing VA and Non-VA Quality of Care: A Systematic Review. J Gen Intern Med. 2017 Jan;32(1):105-121. doi: 10.1007/s11606-016-3775-2. Epub 2016 Jul 15. PMID: 27422615; PMCID: PMC5215146.
- Rasmussen P, Farmer CM. The Promise and Challenges of VA Community Care: Veterans’ Issues in Focus. Rand Health Q. 2023 Jun 16;10(3):9. PMID: 37333666; PMCID: PMC10273892.
