But Costs Were Higher Than Community Care

Cutting-Edge Care at VAMCs: Vivek Jagadale, MD, performs total knee replacement surgery on a veteran while utilizing a Mako SmartRobotics System at the North Florida / South Georgia Veterans Health System’s Malcom Randall VAMC in Gainesville, FL. Robotic surgery has reduced length-of-stay, patient pain and time in physical therapy. Photo from the North Florida/ South Georgia Veteran Health System.
MENLO PARK, CA — Outcomes were better for some common conditions among veterans treated in VA hospitals compared to community care, but the tradeoff often was higher resource use.
A That’s according to a study led by the VA Palo Alto, CA, Health Care System compared outcomes at VA hospitals and non-VA hospitals for six conditions for veterans younger than 65 years and those 65 years and older.
“In this cohort study of 593,578 hospitalizations and 414,861 patients, VA hospitalizations compared with non-VA hospitalizations had significantly lower 30-day mortality for heart failure and stroke, lower 30-day readmission for coronary artery bypass graft, gastrointestinal hemorrhage, heart failure, pneumonia, and stroke, but longer mean length of stay and higher mean costs for most conditions,” the authors pointed out, although there were differences by age group. The results were published in JAMA Network Open.1
Thanks to the Veterans Access, Choice and Accountability Act (Choice Act) in 2014, followed by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act in 2018, which expanded the criteria to purchase care for veterans experiencing access barriers, many veterans enrolled in the VA healthcare system have access to non-VA care through insurance and VA-purchased community care.
While previous comparisons of VA and non-VA hospital outcomes have been limited to subpopulations, this study team—which included participants from the VA Salt Lake City, UT, Health Care System and several academic institutions—sought to compare outcomes for six acute conditions in VA and non-VA hospitals for younger and older veterans using VA and all-payer discharge data.
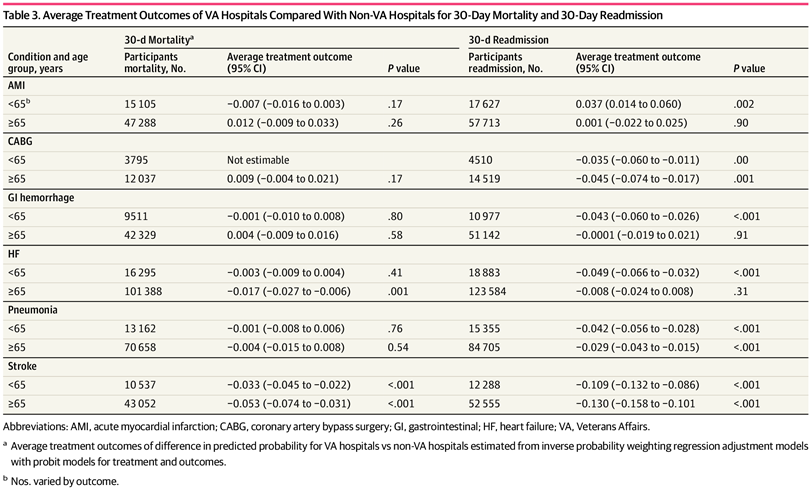
Click to Enlarge: Average Treatment Outcomes of VA Hospitals Compared With Non-VA Hospitals for 30-Day Mortality and 30-Day Readmission Source: JAMA Network Open
The cohort study used a repeated cross-sectional analysis of hospitalization records for:
- acute myocardial infarction (AMI),
- coronary artery bypass graft (CABG),
- gastrointestinal (GI) hemorrhage,
- heart failure (HF),
- pneumonia and
- stroke.
The participants were VA enrollees from 11 states at VA and non-VA hospitals from 2012 to 2017. Analysis was conducted from July 1, 2022, to Oct. 18, 2023.
The researchers focused on 30-day mortality, 30-day readmission, length of stay (LOS) and costs. The patients had a mean age of 75 and were 98% male. Included in the analysis were 442,297 hospitalizations of non-Hispanic white patients (75%) and 73,155 hospitalizations of non-Hispanic Black patients (12%) overall.
Results indicated that VA hospitalizations had a lower probability of 30-day mortality for HF (age ≥65 years, −0.02 [95% CI, −0.03 to −0.01]) and stroke (age <65 years, −0.03 [95% CI, −0.05 to −0.02]; age ≥65 years, −0.05 [95% CI, −0.07 to −0.03]).
VA hospitalizations had a lower probability of 30-day readmission for CABG (age <65 years, −0.04 [95% CI, −0.06 to −0.01]; age ≥65 years, −0.05 [95% CI, −0.07 to −0.02]), GI hemorrhage (age <65 years, −0.04 [95% CI, −0.06 to −0.03]), HF (age <65 years, −0.05 [95% CI, −0.07 to −0.03]), pneumonia (age <65 years, −0.04 [95% CI, −0.06 to −0.03]; age ≥65 years, −0.03 [95% CI, −0.04 to −0.02]), and stroke (age <65 years, −0.11 [95% CI, −0.13 to −0.09]; age ≥65 years, −0.13 [95% CI, −0.16 to −0.10]) but higher probability of readmission for AMI (age <65 years, 0.04 [95% CI, 0.01 to 0.06]).
“VA hospitalizations had a longer mean LOS and higher costs for all conditions, except AMI and stroke in younger patients,” the researchers advised.
Increased Use of Non-VA Care
The VA healthcare system is the only nationally integrated delivery system in the United States, according to background information in the article. In addition to legislation opening up more community care for veterans, the Patient Protection and Affordable Care Act further expanded access to Medicaid for low-income adults, including veterans, in many states beginning in 2014. One result of those policies was increased use of non-VA care and decreased use of VA services.
“Increased access to non-VA care can lead to better outcomes if patients receive higher-quality or more timely care,” the authors explained. “However, studies comparing quality of VA and private clinicians documented process and outcome measures for VA care that were equivalent to or superior to non-VA care for surgical procedures, some hospital care, and preventive care. Many of these prior studies were limited to older veterans using VA services and older patients using Medicare services, including many nonveterans, due to wide availability of Medicare data.”
Yet, the researchers pointed out that the veteran-enrollee population is more male and has worse health status, greater disability and lower incomes compared with the nonveteran population. “Moreover, younger veterans are typically not included in comparisons due to a lack of comprehensive data on non-VA use outside of Medicare, which reduces the generalizability of these comparisons,” they wrote. “Other studies compared VA and community care purchased by the VA and focused on select subpopulations having a particular condition or receiving a particular procedure.”
For this study, the researchers used a comprehensive data set of VA and non-VA all-payer inpatient care records, adding, “No studies to date compared hospital outcomes for veterans of all ages with access to VA care.”
“After accounting for selection of patients into VA or non-VA hospitals, patients treated in VA hospitals had significantly lower probability of 30-day mortality than those in non-VA hospitals for HF among older patients and stroke for both younger and older patients,” the study reported. “Patients treated for CABG, GI hemorrhage, HF, pneumonia, and stroke in VA hospitals had lower probability of readmission compared with patients in non-VA hospitals; however, differences for GI hemorrhage and HF were found only in younger patients. In contrast, younger patients hospitalized for AMI in VA hospitals had higher probability of readmission than non-VA patients.”
They spotlight that mean hospitalization costs were mostly higher and that mean LOS was longer in VA hospitals for the study conditions. In the case of AMI hospitalizations, however, costs for younger patients were lower in VA hospitals than non-VA hospitals.
“Our findings showing lower mortality in VA hospitals for 2 of the 6 conditions suggests that there was a mortality advantage associated with VA hospitals but not for all types of care,” the authors stated. “Recent studies of inpatient surgery and emergency department care also found associations between lower mortality and better quality in VA hospitals compared with non-VA hospitals. More research is needed to determine what aspects of VA care, such as post discharge care, can improve mortality and whether there are differences for other clinical outcomes.”
The study suggested that VA hospitals might be better at reducing readmissions due to an integrated delivery system, implementation of the patient-centered medical home and an electronic medical record system.
As to why mean LOS was longer and costs were higher in VA hospitalizations for most conditions compared with non-VA hospitalizations, the researchers posited that, because Medicare and private insurance payment policies, such as bundled payment programs, have focused on efficiency, that could have spurred hospitals to discharge patients sooner while VA hospitals were unaffected by such policies. That might have allowed VA hospitals to keep patients longer to ensure they are stable before discharging them, they suggested.
“Expanding access to non-VA care may improve timeliness and reduce travel costs for many veterans; however, there are tradeoffs with higher mortality and readmissions in non-VA hospitals observed across age groups,” the study team concluded. “As more veterans use care in the community paid for by the VA due to the MISSION Act, our findings suggest there may be reasons for concern. Veterans could experience worse outcomes for some types of care without well-developed community care networks based on quality standards and sufficient care coordination between VA and non-VA clinicians. In an era of greater choice, veterans’ often benefit by choosing VA care.”
- Yoon J, Phibbs CS, Ong MK, et al. Outcomes of Veterans Treated in Veterans Affairs Hospitals vs. Non-Veterans Affairs Hospitals. JAMA Netw Open. 2023;6(12):e2345898. doi:10.1001/jamanetworkopen.2023.45898

