Trend Continues With 16% Drop Since 2020
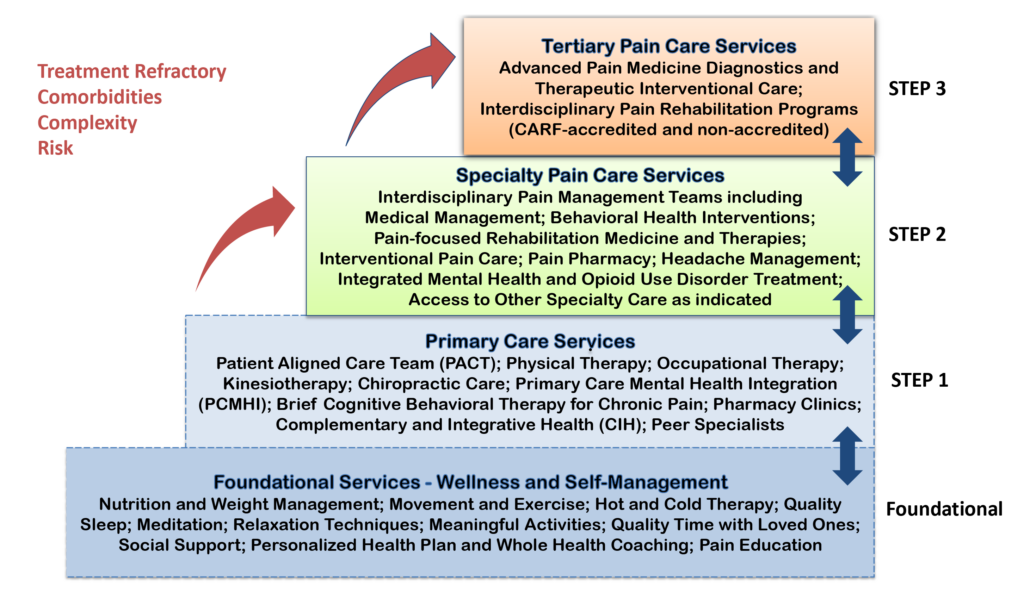
Click to Enlarge: VHA is improving pain care through implementation of the Stepped Care Model for Pain Management (SCM-PM). Source: VA
WASHINGTON, DC — The number of VHA patients with opioid prescriptions has plummeted by 67% since 2012, primarily because of the agency’s Opioid Safety Initiative (OSI) beginning a decade ago.
The VA announced that 288,820 veterans had opioid prescriptions in 2023, compared to 874,897 in 2012.
The nation’s largest integrated healthcare system described in a press release how it has adopted a so-called whole-health approach to veteran-centered pain care, which focuses on the patient as a whole person and provides evidence-based treatment using interdisciplinary pain management teams instead of only relying on one treatment, such as painkillers.
Part of the process is having veterans complete a personal health inventory self-assessment and the creation of personal health plan. The VA also offers courses to help patients learn about whole health practice and take charge of their lives and health.
Another key element is the VA’s Stepped Care Model for Pain Management. A foundational program includes nutrition and weight management, movement and exercise, quality sleep and relaxation techniques delivered through a personalized health plan and supported by whole-health coaches. Other aspects of the model involve using alternative medications to opioids and taking advantage of complementary medical techniques.
“More than a third of veterans who use VA live with chronic pain, so it’s a top priority for us to help them manage that pain safely and effectively,” said VA’s Under Secretary for Health Shereef Elnahal, MD. “By providing comprehensive pain-management tools, we can often avoid the need for potentially addictive medications or invasive procedures. Our goal is to help veterans live full, meaningful, pain-free lives—and we will continue to look for new ways to help veterans do exactly that.”
VA’s OSI began in 2013. VA credits the following for leading to its success:
- significant investment in interdisciplinary pain management teams,
- a sustained focus on increasing access to proven therapies and treatments, and
- updating opioid treatment guidelines and implementing best practices.
At the same time, the number of patients receiving opioids and benzodiazepines together dropped by 90%, from 162,444 in 2012 to 15,981 in 2023, reducing the number of patients on long-term opioid medications by 71%, from 569,207 in 2012 to 162,261 in 2023 and lowering the number of patients on high doses of opioids by 81%, from 76,444 in 2012 to 14,733 in 2023.
Most veterans who still receive opioid prescriptions from the VHA have prescriptions for short-term pain care, such as for surgery or an injury. For patients on long-term opioid therapy for chronic pain conditions, VA uses a patient-centered approach that treats and monitors each veteran individually according to their needs.
The overall number of opioid-users also has dropped 16% since 2020, the last time VA publicly reported the numbers. In addition, since 2020, VA has reduced the number of patients receiving opioids and benzodiazepines together by 26%, the number of patients on long-term opioids by 27% and the number of patients on high doses of opioids by 19%.
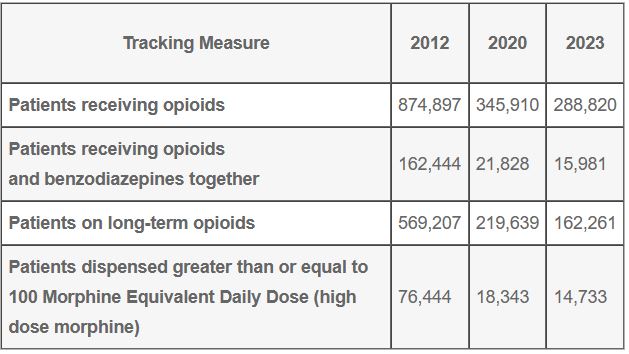 The 2012 and 2020 numbers below have been updated from the previous release due to a change in Centers for Disease Control and Prevention tracking measures:
The 2012 and 2020 numbers below have been updated from the previous release due to a change in Centers for Disease Control and Prevention tracking measures:
Veteran pain care at VA is broadly divided into five categories, including medication, restorative therapies, interventional procedures, behavioral health approaches, and complimentary and integrative health.
Recent Update
Earlier this year, a review of updated VA/DoD guidelines called for new measures to reduce the use of opioid pain relievers in the management of chronic pain, including the preferential use of buprenorphine over full agonist opioids.
The 2022 updated guideline also urged physicians to assess for behavioral health risk when considering prescribing opioids, including screening patients with acute pain for pain catastrophizing, such as anticipating that pain will last an extended period of time. It also suggested that clinicians offer education before surgery to help reduce the risk of opioid painkillers’ overuse during the recovery period.
Many of the previous recommendations were confirmed by the latest guideline development group, including not recommending the use of opioids in the daily management of chronic pain because the benefits are small and outweighed by risks to the patient. If opioids are required, they write, the lowest possible dose for the shortest amount of time should be used.
A synopsis of the guidelines, approved last year by VA and DoD leadership, appeared in February in the Annals of Internal Medicine. The authors said the report highlighted the recommendations they considered most important.1
In December 2020, the VA/DoD Evidence-Based Practice Work Group put together a team to update the 2017 VA/DoD Clinical Practice Guideline for Opioid Therapy for Chronic Pain.
“Chronic pain is a common, costly, and disabling medical condition in the United States,” according to background information in the synopsis. “It has been estimated that nearly 50 million adults experience chronic pain on most days or every day pain is also associated with approximately 20% of all ambulatory primary care and specialty visits in the United States.”
The report recounted how, beginning in the late 1990s until 2008, there was a significant increase in prescribing of opioids for pain relief—and an accompanying jump in opioid-related morbidity and mortality, overdose death and admissions for treatment of substance use disorder. Since then, the VA and DoD have been at the forefront of trying to reduce overuse of opioid pain medications.
The guideline panel included practicing clinicians in a range of specialties, including internal medicine, family medicine, neurology, nursing, pharmacy, psychology, physical therapy, social work, acupuncture and Chinese medicine and chiropractic and interventional medicine.
Among the key changes from the previous 2017 document, in addition to those listed above, is that treatment algorithms, which help guide clinicians through decision-making processes, have been updated and condensed so that there are now 3 rather than 4, as in the previous 2017 guideline.
As in past guidelines, the recent panel recommended against the initiation of opioid therapy for the management of chronic noncancer pain. “Compared with the 2017 recommendation against initiation of long-term opioid therapy, the updated recommendation against opioid therapy in general for chronic pain is broader and reflects the evidence that opioid therapy for any duration may be harmful,” according to the authors. Citing recent research used in developing the new guidelines, they added, “Although opioids can improve pain severity and functional status in some patients with musculoskeletal pain, including chronic low back pain and osteoarthritis in studies of 4 to 24 weeks’ duration, the effects are small, are accompanied by adverse events, and are generally believed to be without important benefit on pain or function.”
- Sandbrink F, Murphy JL, Johansson M, et al; VA/DoD Guideline Development Group. The Use of Opioids in the Management of Chronic Pain: Synopsis of the 2022 Updated U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline. Ann Intern Med. [Epub 14 February 2023]. doi:10.7326/M22-2917
