Study Strongly Recommends Routine Liver Testing for Patients
Click to Enlarge: Abbreviations: AUDIT-C, Alcohol Use Disorders Identification Test; FIB-4, Fibrosis-4. Source: JAMA Network Open
RICHMOND, VA — Could 1 in 10 veterans diagnosed with dementia actually have reversible cognitive decline caused by advanced liver disease?
A new analysis from the Virginia Commonwealth University’s School of Medicine and the Richmond, VA, VAMC suggested that could be the case.
The study in JAMA Network Open pointed out the difficulties for clinicians to differentiate dementia from the cognitive decline caused by hepatic encephalopathy, often called cirrhosis. Yet, if undetected, patients might not receive appropriate treatment that can reverse or halt the impairment.
The authors recommended that physicians treating veterans with dementia should consider assessing their patients for liver disease to make sure cirrhosis isn’t to blame.
“This unexpected link between dementia and liver health emphasizes the importance of screening patients for potentially treatable contributors to cognitive decline,” said lead author Jasmohan Bajaj, MD, of VCU and the Richmond VAMC.
The retrospective cohort study included 177,422 veterans with a diagnosis of dementia. A high Fibrosis-4 score suggestive of advanced liver fibrosis to cirrhosis was observed in 5% to 10% of the patients who previously did not have a diagnosis of cirrhosis. The findings were supported by two validation cohorts within the Richmond VAMC.
“The findings of this study suggest that clinicians treating patients with dementia should investigate a reversible factor associated with cognitive decline, including missed or undiagnosed cirrhosis with hepatic encephalopathy,” the researchers emphasized.
The study was conducted between 2009 and 2019 using data from the VHA, with data analysis conducted from May 20 to Oct. 15, 2023. Participants, 0.1% men; 80.7% white and with a mean age of slightly more than 78, had a diagnosis of dementia at two or more clinic visits, no prior diagnosis of cirrhosis and came with sufficient laboratory test results to calculate the Fibrosis-4 (FIB-4) score.
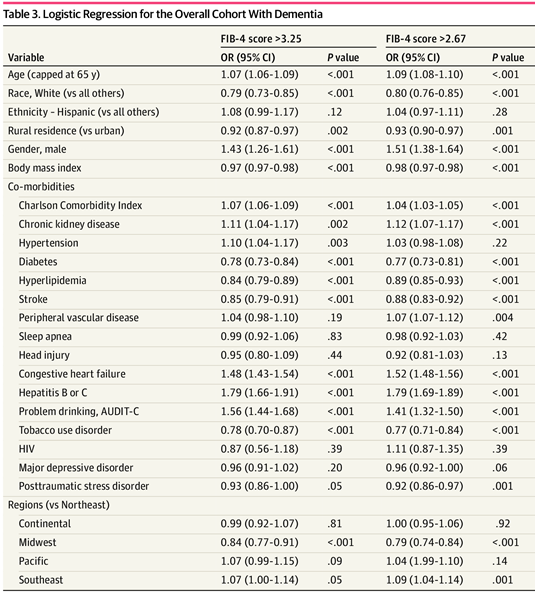
The researchers were focused on the FIB-4 score (>2.67 suggestive of advanced fibrosis and >3.25 suggestive of cirrhosis), capped at age 65 years, even for those above this cutoff who were included in the analysis.
The results indicated that 5.3% (n = 9373) had an FIB-4 score greater than 3.25 and 10.3% (n = 18 390) had an FIB-4 score greater than 2.67. “In multivariable logistic regression models, FIB-4 greater than 3.25 was associated with older age (odds ratio [OR], 1.07; 95% CI, 1.06-1.09), male gender (OR, 1.43; 95% CI, 1.26-1.61), congestive heart failure (OR, 1.48; 95% CI, 1.43-1.54), viral hepatitis (OR, 1.79; 95% CI, 1.66-1.91), Alcohol Use Disorders Identification Test score (OR, 1.56; 95% CI, 1.44-1.68), and chronic kidney disease (OR, 1.11; 95% CI, 1.04-1.17),” according to the report.
That score was inversely associated with white race (OR, 0.79; 95% CI, 0.73-0.85), diabetes (OR, 0.78; 95% CI, 0.73-0.84), hyperlipidemia (OR, 0.84; 95% CI, 0.79-0.89), stroke (OR, 0.85; 95% CI, 0.79-0.91), tobacco-use disorder (OR, 0.78; 95% CI, 0.70-0.87) and rural residence (OR, 0.92; 95% CI, 0.87-0.97).
“Similar findings were associated with the FIB-4 greater than 2.67 threshold. These codes were associated with cirrhosis on local validation,” the authors noted. “A local validation cohort of patients with dementia showed a similar percentage of high FIB-4 scores (4.4%-11.2%).”
Background information in the article discussed how dementia poses a major clinical, psychosocial, and financial burden worldwide and also has a suboptimal therapeutic landscape. On the other hand, metabolic encephalopathies, such as hepatic encephalopathy (HE), are reversible with therapy, “although their diagnosis requires a high index of suspicion.”
Liver Disease Often Undiagnosed
The researchers further noted that “major changes in the epidemiologic factors of liver disease are attributed to widespread advances for viral hepatitis care, with increasing rates of metabolic syndrome and alcohol use disorder (AUD). However, a substantial proportion of advanced liver disease remains undiagnosed, especially among US veterans, who have major risk factors for both cirrhosis and dementia.”
The study pointed out that many veterans receiving VA care are aging and often have comorbid conditions that affect cognitive function, such as AUD, posttraumatic stress disorder (PTSD) and head injuries, in addition to risk factors for cirrhosis.
“Among veterans with cirrhosis, concomitant dementia is common and is challenging to distinguish from HE, but the extent to which patients with diagnoses of dementia also have undiagnosed cirrhosis and HE is unknown,” the authors wrote. “Undiagnosed cirrhosis among veterans with dementia could raise the possibility that part of their cognitive impairment may be due to reversible HE. Therefore, the determinants of undiagnosed cirrhosis among veterans with dementia is important to identify those eligible for screening and subsequent HE therapy.”
“Early detection of liver issues allows for targeted interventions and opens avenues for addressing treatable factors contributing to cognitive decline,” Bajaj said in a VCU press release.
Hepatic encephalopathy is a nervous-system disorder brought on by cirrhosis. Suboptimal liver function allows toxins to build up in the blood and travel to the brain, causing confusion and delirium. Widely available medications can rid the body of toxins and reverse the process, however, according to the report.
Bajaj said the study was initiation after the cases of two older men who were thought to have dementia and Parkinson’s disease, but whose symptoms dramatically improved after being treated for hepatic encephalopathy. In a study published a year ago in the American Journal of Gastroenterology, Bajah and colleagues published findings that dementia is commonly diagnosed in patients with cirrhosis and correlates with a diagnosis of HE, independent of alcohol use, brain injury, age and other metabolic risk factors.2
To further information on the issue, the authors of the new study looked at a large cohort of U.S. veterans receiving care nationwide. The study pointed out that factors that increase the risk of cirrhosis include older age, being male, congestive heart failure, viral hepatitis, alcohol use and certain health conditions.
Among other findings, the data indicated that dementia disproportionately affected Black and Hispanic veterans and that they were more likely to be diagnosed later in the disease course. Non-Hispanic white veterans who did not use tobacco or had diabetes were less likely to have elevated FIB-4 scores.
“The next step is to ensure that healthcare providers taking care of patients with cirrhosis and well as those with dementia are made aware of a potential overlap with hepatic encephalopathy, which is treatable,” Baja said. “Routinely using the FIB-4 index to evaluate dementia could help a significant number of patients, families and physicians by providing an opportunity to treat and potentially reverse cognitive impairment brought on by liver disease,” he added.
- Bajaj JS, Silvey SG, Rogal S, et al. Undiagnosed Cirrhosis and Hepatic Encephalopathy in a National Cohort of Veterans With Dementia. JAMA Netw Open. 2024;7(1):e2353965. doi:10.1001/jamanetworkopen.2023.539652.
- Adejumo A, Noll A, Rogal S, Yakovchenko V, et. Al. Dementia Frequently Coexists With Hepatic Encephalopathy but Not Other Cirrhosis Complications in US Veterans. The American Journal of Gastroenterology 118(3):p 475-480, March 2023. | DOI: 10.14309/ajg.0000000000002189

