Brain Appears to Be Affected By Electric Signals
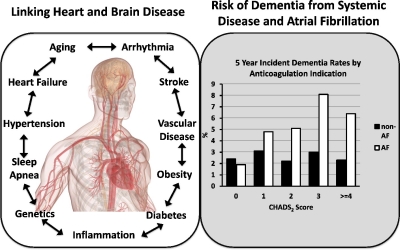
Atrial fibrillation incrementally increases dementia risk across all CHADS2 and CHA2DS2VASc strata in patients receiving long-term warfarin.
SAN FRANCISCO — The most feared consequence of atrial fibrillation has long been ischemic stroke, but the erratic heartbeat doesn’t just raise the risk that a blood clot formed in the heart will lodge in the brain with sudden and frequently fatal results. Increasingly, it appears that the chaotic electric signals generated in the heart also causes longer-term, cumulative damage to the brain that can be just as devastating.
Over the last decade, a growing body of research has noted an association between AF and cognitive impairment and dementia, including Alzheimer’s disease. The VA cares for one in 10 Americans with atrial fibrillation (AF), making understanding the impact of atrial fibrillation on brain health a matter of critical importance to the department.
More than 1.2 million veterans have a diagnosis of atrial fibrillation today. That number is expected to continue to rise as the veteran population ages; atrial fibrillation occurs at six times the rate in individuals over the age of 65 as in the general population and half of patients with AF are at least 80 years of age. Obesity, diabetes, heavy alcohol use, hypertension, and chronic kidney disease—all common among veterans—also substantially increase the risk of atrial fibrillation.
Individuals with AF have an irregular and often rapid heart rate caused by misfiring electrical signals that stimulate the atria to beat out of sync with the ventricles. While many individuals have no indication they have AF, others experience heart palpitations, shortness of breath and general weakness.
Teasing out the exact nature and magnitude of the association between AF and dementia has proved challenging. Some studies have linked cognitive decline with management of anticoagulation in AF, while others have concluded that the severity of AF is the critical factor rather than choice of anticoagulant. Others have evaluated the association over a relatively short period of time and in small populations, raising questions about the generalizability of the findings and the efficacy of interventions.
Veterans, AF and Dementia
Given the prevalence of AF among veterans and the impact an association with dementia would have on their care, researchers at the San Francisco VAMC, the University of California-San Francisco, and the Northern California Institute for Research and Education sought to elucidate the links between AF, anticoagulation, cognitive decline and dementia. To do so, they analyzed the records of 407,871 veterans over age 55 who received care through the VHA between August 2003 and September 2015.1
In a study recently published in the American Journal of Geriatric Psychiatry, they hypothesized that the association between AF and dementia could be driven by the increased risk of ischemic stroke and transient ischemic attacks. Further, they wanted to better understand the risk of dementia specifically in veterans with AF, given their higher risk of dementia as a result of military-related risk factors as well as cardiovascular disease.
Veterans were included in the group with incident AF if they had a first diagnosis of the condition and at least one subsequent documented diagnosis as part of routine clinical care during a four-year baseline period. On that basis, 16,382 veterans had newly diagnosed AF. Veterans with AF were more likely to also have comorbidities such as hypertension, diabetes, obesity, myocardial infarction, chronic heart failure, transient ischemic attacks or stroke, and valvular heart disease. Veterans with AF were also far more likely to take anticoagulants, 44.1% vs. 1.7% of those without AF.
In the group with AF, those prescribed anticoagulants were significantly younger and more likely to be Black than those who did not receive the drugs. They also had significantly higher rates of hypertension, diabetes, obesity, and cardiovascular or cerebrovascular disease.
The team found that AF increased the odds of developing dementia by 14% overall. Chronic heart failure mediated the association between AF and dementia by 21% while valvular heart disease, TIA/stroke, and myocardial infarction mediated that association by 13%, 12%, and 10%, respectively.
“Our findings add to the literature that veterans with atrial fibrillation are more likely to develop dementia compared to those without atrial fibrillation, and that this association is partially mediated by TIA/stroke and cardiovascular disease,” the researchers wrote. Based on their findings, the researchers recommended that “patients with AF should be periodically screened for dementia, and ongoing and future treatment trials should also consider including dementia among the outcomes assessed.”
The Atherosclerosis Risk in Communities Neurocognitive Study (ARIC-NCS) reached similar conclusions in its analysis of data from 12,515 participants in a community cohort over a 20-year period. In that study, incident AF increased the risk of dementia by 23%, after adjustment for stroke and other cardiovascular risk factors.
Like VA/UCSF researchers, the ARIC-NCS team urged greater attention to cognitive function in AF patients, noting that “[B]ecause cognitive decline is a precursor to dementia, our findings prompt further investigation to identify specific treatments for AF that will delay the trajectory of cognitive decline and, thus, prevent dementia in patients with AF.”
Anticoagulant Impact
The veterans with AF who took anticoagulants had 44% greater odds of later dementia compared to veterans with AF who did not use the blood thinners, “likely due to indication bias of greater AF severity,” the team concluded.
The choice of anticoagulant could also be a factor, however, as other studies have found that direct acting oral anticoagulants (DOACs) are not associated with the same risk of dementia as warfarin. The researchers did not analyze the risk of dementia by type of anticoagulant. Notably, for most of the period studied, veterans who received anticoagulants were prescribed warfarin. In 2011, the first year DOACs were approved for use in the VA, just 2% of patients with AF received them, while nearly 45% received warfarin. As of 2015, the final year of the study, DOAC use remained below 15%.
A direct comparison of the choice of anticoagulant on dementia found DOACs reduced the risk by 15% to 20% in a study population of more than 468,000. “Our findings suggest the following: (1) DOACs may be superior to warfarin with respect to outcome of dementia, which is considered as an important adverse outcome of AF; and (2) future risk of dementia does not appear to be influenced by choice of DOAC. Therefore, DOAC choice should be driven by other efficacy, safety, and preference considerations,” wrote corresponding author Alvaro Alonso, MD, PhD, with Emory University, and colleagues in a study published in the Journal of the American Heart Association.3
Regardless of the choice of anticoagulant, the study in veterans makes clear that healthcare providers should look for development of cognitive issues in AF patients. The researchers recommended that “patients with AF should be periodically screened for dementia, and ongoing and future treatment trials should also consider including dementia among the outcomes assessed.”
- Rouch L, Xia F, Bahorik A, Olgin J, Yaffe K. Atrial Fibrillation is Associated With Greater Risk of Dementia in Older Veterans. Am J Geriatr Psychiatry. 2021 Feb 9:S1064-7481(21)00205-0. doi: 10.1016/j.jagp.2021.02.038. Epub ahead of print. PMID: 33663986.
- Chen LY, Norby FL, Gottesman RF, Mosley TH, Soliman EZ, Agarwal SK, Loehr LR, Folsom AR, Coresh J, Alonso A. Association of Atrial Fibrillation With Cognitive Decline and Dementia Over 20 Years: The ARIC-NCS (Atherosclerosis Risk in Communities Neurocognitive Study). J Am Heart Assoc. 2018 Mar 7;7(6):e007301. doi: 10.1161/JAHA.117.007301. PMID: 29514809; PMCID: PMC5907543.
- Chen N, Lutsey PL, MacLehose RF, Claxton JS, Norby FL, Chamberlain AM, Bengtson LGS, O’Neal WT, Chen LY, Alonso A. Association of Oral Anticoagulant Type With Risk of Dementia Among Patients With Nonvalvular Atrial Fibrillation. J Am Heart Assoc. 2018 Nov 6;7(21):e009561. doi: 10.1161/JAHA.118.009561. PMID: 30571385; PMCID: PMC6404188.
- Am Heart J. 2017 Jun;188:93-98. doi: 10.1016/j.ahj.2017.02.026. Epub 2017 Feb 24. PMID: 28577686.
