Veterans’ Study Looked at Effects of Extreme Weather
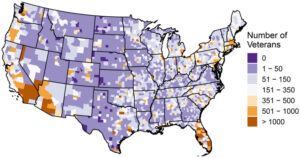
Click to Enlarge: County level totals of deceased veterans with COPD (2016 to 2021, n=377,545) in the VHA health care system based on county of residence at time of death. The map was created using R statistical software. Note: COPD, chronic obstructive pulmonary disease; VHA, Veterans Health Administration. Source: Environmental Health Perspectives
MINNEAPOLIS — Patients with chronic obstructive pulmonary disease (COPD) are adversely impacted by extreme weather conditions, and the effects vary by gender and ethnic backgrounds.
A new report in Environmental Health Perspectives discussed environmental disturbances, including heat and cold waves, that can exacerbate disease symptoms in the U.S. veteran population.1
Researchers from the University of Minnesota School of Public Health and the Minneapolis VA Healthcare System pointed out that the weather conditions increased the risk of all-cause mortality in COPD patients, with cold waves conferring a greater number of excess deaths compared to heat waves.
“Cisgender women were estimated to have greater risks of mortality due to heat wave exposure, with suggestive evidence of elevated heat wave risk in Black veterans,” the study team wrote. “AIAN [American Indian/Alaska Natives] and Hispanic veterans may have elevated risk due to cold wave exposure. This study elucidated the impacts of heat and cold waves among a population of veterans with a chronic respiratory disease, and these results can inform future clinical treatment and public health policy to lessen the burden of climate-related hazards in high-risk populations.”
For the study, investigators collected individual level data with geocoded residential addresses from the VHA on 377,545 deceased patients with COPD from 2016 to 2021. The time stratified case-crossover study was designed to estimate the incidence rate ratios (IRR) of heat and cold wave mortality risks using conditional logistic regression models examining lagged effects up to seven days.
The results indicated that heat waves had the strongest effect on all-cause mortality at lag day 0 [IRR: 1.04; 95% confidence interval (CI): 1.02, 1.06] with attenuated effects by lag day 1. The AR at lag day 0 was 651 (95% CI: 326, 975) per 100,000 veterans, the authors advised.
Meanwhile, the effect of cold waves steadily increased from lag day 2 and plateaued at lag day 4 (IRR: 1.04; 95% CI: 1.02, 1.07) with declining but still elevated effects over the remaining 7-day lag period,” they noted. “The AR at lag day 4 was 687 (95% CI: 344, 1,200) per 100,000 veterans. Differences in risk were also detected upon stratification by gender and race.”
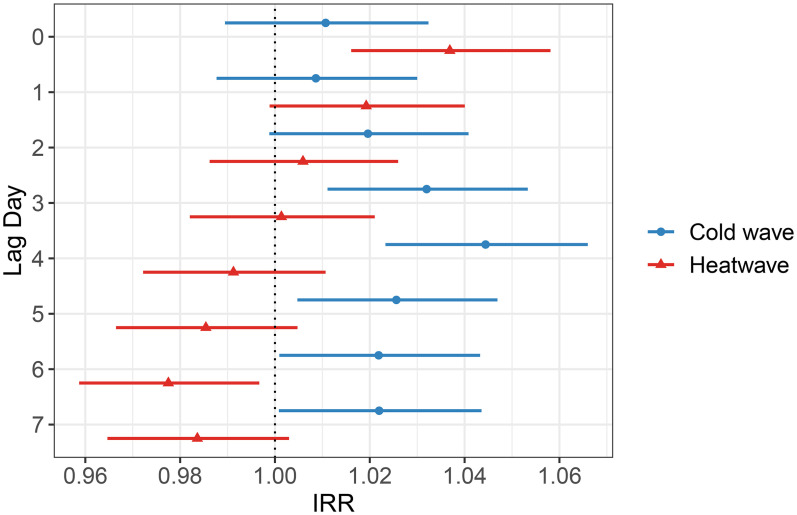
Click to Enlarge: The estimated incidence rate ratio (IRR) for heat and cold wave associations with all-cause mortality among veterans with COPD (2016 to 2021, n=377,545) from lag day 0 to 7. Heat waves, defined as 2+ consecutive days where the ambient mean daily temperature exceeded the 90th percentile of ambient mean temperature values for the warm season (April to September) from 1992 to 2021. Cold waves, defined as 2+ consecutive days where the ambient mean daily temperature was below the 10th percentile of ambient mean temperature values for the cold season (October to March) from 1992 to 2021. Estimates (95% CIs) were generated via conditional logistic regression models adjusted for daily total precipitation, mean wind speed, mean specific humidity, and holiday status. Points represent the estimated IRR and lines denote the 95% CI of the estimated IRR. Numeric data can be found in Table S3. Note: CI, confidence interval; COPD, chronic obstructive pulmonary disease. Source: Environmental Health Perspectives
The authors urged that future research should further estimate the associations between extreme weather events and health outcomes for high-risk populations with chronic medical conditions.
The issue is of special concern, they pointed out, because of climate change. “Anthropogenic climate change is causing harmful planetary effects with increased frequency, intensity, duration, and geographic extent of extreme weather events, including heat waves, droughts, wildfires, and floods,” according to their report. “Furthermore, climate change disproportionately affects children, the elderly, racial minorities, impoverished communities, and those living with underlying comorbidities such as chronic obstructive pulmonary disease (COPD).”
Background information in the article defined COPD as a heterogeneous, degenerative pulmonary disease characterized by airflow obstruction, which affects around 6% of the adult population.
“While the overall age adjusted mortality rates of COPD in the United States decreased in recent decades, improvements in COPD mortality were not equally distributed among the population,” the authors explained. “Age-adjusted mortality rates in males have decreased over time, but age-adjusted mortality rates in females remained relatively unchanged. African American women were the only race-sex combination that had an increase in age-adjusted mortality rates from 2004 to 2018.”
Environmental Perturbations
They added that COPD patients “are often more susceptible to environmental perturbations due to compromised respiratory health and high rates of comorbidities, which lead to further debilitation and poorer health.”
Extremes in ambient temperature, both heat and cold, are known to increase the risk of general mortality. Little individual level evidence is available, however, on how heat and cold waves impacts populations with underlying chronic disease, however.
In general, they wrote that heat waves had an immediate impact on all-cause mortality, while cold wave effects demonstrated a delayed response starting on lag day 2, with the greatest effect detected at lag day 4 for most populations, noting, “Within specific subpopulations, the effect of heat waves was larger in women than in men and in black veterans than in white veterans. Of note, the effect of cold waves was greater in AIAN and Hispanic veterans compared to white and non-Hispanic veterans, respectively.”
The researchers posited that one potential explanation for the disparate responses in heat and cold wave effects might be related to the underlying cause of death. “Heat waves are predominately associated with more acute causes of death, such as cardiovascular dysfunction or heat stress,” they stated.
The study team also posited a direct impact of extreme heat on the respiratory system, although it is not completely clear extreme heat impacts COPD. “Among individuals with asthma, research suggested inhalation of hot and humid air may induce bronchoconstriction mediated via the cholinergic reflex,” the article suggested.
The underlying delayed effects of cold waves on health risks and the biological mechanisms underlying them are even less understood, according to the study, and likely are associated with more subacute causes of death, such as COPD exacerbations.
“In a population of individuals with COPD, delayed impacts of cold wave–associated mortality may be attributed to viral respiratory infections and bacterial pneumonia, both more common in the cold season of the year,” the researchers proposed. “Higher rates of adverse COPD-related outcomes, including exacerbations and hospitalizations, in the cold season is another well-documented phenomenon that may explain our results. Inflammation and bronchoconstriction are two postulated mechanisms by which cold exposure negatively affects individuals with COPD.”
The report emphasized that both heat waves and cold waves conferred a similar absolute risk of mortality on their strongest lag days in the veteran population with 651 deaths per 100,000 attributable to heat wave lag day 0 exposure and 687 deaths per 100,000 attributable to cold wave lag day 4 exposure, respectively.
The study’s age stratified estimates didn’t detect differences between older and younger veterans in the cohort, in contrast to other research that has found age–related disparities in both heat and cold wave–associated mortality. “Indeed, a recent review concluded strong evidence for higher mortality risk in older populations due to extreme heat and cold exposure attributed to physiology, behavioral practices, prevalence of comorbidities, living alone, and access to indoor heat and air conditioning,” the authors explained. “Furthermore, it would be hypothesized that as a veteran aged and transitioned into a retirement phase, living conditions, behaviors, and physical health would change, which could enhance susceptibility to extreme weather events, but this has not been formally tested. The lack of disparate mortality risk between the age groups in our study could, however, be reflective of the quality and access of care received at the VHA.”
- Rau A, Tarr GAM, Baldomero AK, Wendt CH, Alexander BH, Berman JD. Heat and Cold Wave-Related Mortality Risk among United States Veterans with Chronic Obstructive Pulmonary Disease: A Case-Crossover Study. Environ Health Perspect. 2024 Feb;132(2):27004. doi: 10.1289/EHP13176. Epub 2024 Feb 9. PMID: 38334741; PMCID: PMC10855215.

