Mortality Rates Higher With Hypnotic Medications
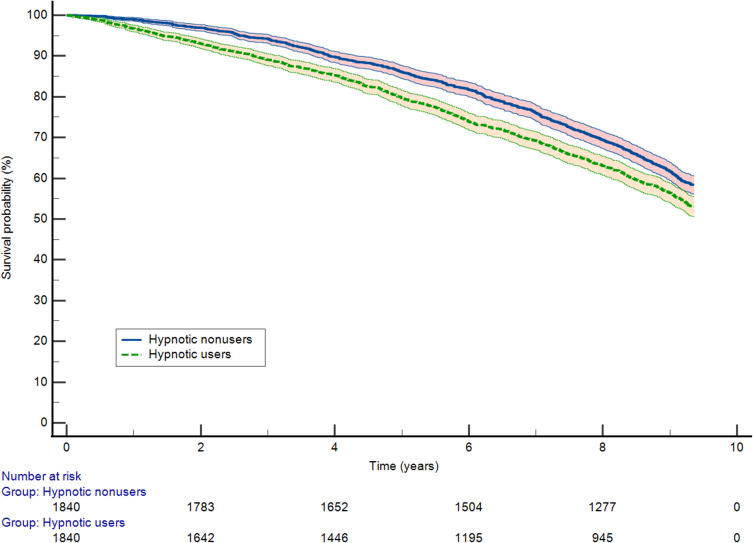
Click to Enlarge: Kaplan–Meier curves for the association between hypnotic use and all-cause mortality in propensity-matched COPD patients with insomnia. Source: International Journal of Chronic Obstructive Pulmonary Disease
BUFFALO, NY — The safety and long-term effects of hypnotic medications in chronic obstructive pulmonary disease (COPD) have been called into question by a new study.
The VA Western New York Healthcare System-led study found a significant association between the use of hypnotics for insomnia and an increased risk of all-cause mortality in patients with COPD. “The risk of death diverges with prolonged use depending on the hypnotic mechanism of action,” according to the authors, who called for further research to establish a causal relationship.
The report in the International Journal of Chronic Obstructive Pulmonary Disease pointed out that hypnotics are commonly prescribed in patients with COPD to manage insomnia. “Given the considerable risks associated with these drugs, the aim of the study was to evaluate the risk of all-cause mortality associated with hypnotics in a cohort of veterans with COPD presenting with insomnia,” the researchers wrote.1
The retrospective cohort study used information from the VHA Corporate Data Warehouse; the data were linked with Medicare, Medicaid, and National Death Index information from 2010 through 2019. All-cause mortality was defined as the primary outcome.
Of 5,759 veterans with COPD included in the study, 3,585 began using hypnotic agents during the investigation period. The veterans had a mean age of 71.7, and 92% were men.
During a mean follow-up of 7.4 (SD, 2.7) years, 2,301 deaths were recorded; of those, 65.2 and 48.7 total deaths per 1,000 person-years occurred among hypnotic users and nonusers, respectively.
After propensity matching, results indicated that hypnotic use was associated with a 22% increased risk of mortality compared with hypnotic nonusers (hazard ratio [HR] 1.22; 95% confidence interval [CI],1.11-1.35).
“The benzodiazepine receptor agonists (BZRAs) group experienced a higher incidence rate of all-cause mortality compared to hypnotic nonusers (Incidence rate ratio [IRR] 1.27; 95% CI, 1.14-1.43),” the researchers advised. “Conversely, the mortality rate of non-BZRA hypnotics decreased after the first 2 years and was not significantly different for hypnotic nonusers (IRR 1.04; 95% CI, 0.82-1.11).”
The study noted that the higher risk of all-cause mortality was observed in patients prescribed BZRAs, with the risk of mortality for non-BZRAs moderating after the first two years, indicating a class effect.
Background information in the report described how, in addition to its pulmonary complications, COPD also often leads to sleep disturbances in patients. The causes include persistent dyspnea, recurrent cough, anxiety and pain.
Treatment Side Effects
“These sleep disturbances have been associated with increased symptom severity, recurrent exacerbations, and poor quality of life,” the authors wrote. “Sleep quality is further aggravated by the side effects of COPD treatment (i.e., β-agonists and corticosteroids). Sleep characteristics include prolonged sleep onset latency, frequent arousals, and lower sleep efficiency.”
The study advised that, according to epidemiologic studies, more than half of COPD patients report insomnia and that coughing and wheezing were especially bothersome.
While cognitive behavioral therapy is considered the first-line treatment for insomnia in COPD patients and often leads to improvement in fatigue and dyspnea, hypnotics are frequently prescribed to improve sleep quality and suppress insomnia. Commonly prescribed drugs include FDA-approved agents for the treatment of insomnia (benzodiazepines, nonbenzodiazepine benzodiazepine receptor agonists (Z-drugs), melatonin receptor agonists, doxepin and dual orexin receptor antagonists (DORAs)) and off-label use medications (trazodone, antipsychotics and anticonvulsants), the study noted.
“The use of these medications comes with associated risks shared with most hypnotics such as next morning residual sleepiness, ataxia, and falls, particularly in elderly COPD patients, and specific to others like benzodiazepine receptor agonists-associated respiratory depression, cognitive impairment, or nocturnal complex behaviors,” the researchers wrote. “The relationship between hypnotic use and mortality in COPD patients is the subject of increasing scientific investigations given the unremitting global rise in disease burden of COPD. Previous studies have raised concerns about increased mortality risks with hypnotics, however, the available evidence is limited and conflicting.”
The authors concluded that, in the cohort of U.S. veterans with COPD and insomnia, the use of hypnotics was found to be independently associated with all-cause mortality, “but this association was more pronounced among older patients and in those who were prescribed BZRA hypnotics. The risk of mortality with non-BZRA hypnotics abated after the first 2 years in comparison to BZRA hypnotics and achieved parity with hypnotic nonusers after 4 years of consumption.”
The issue, according to the researchers, is that hypnotic agents produce significant improvements in total sleep time, subjective sleep latency and frequency of arousals during sleep, but they also can cause a range of respiratory and nonrespiratory side effects, including worsening apneas, severe nocturnal desaturations, frequent exacerbations, respiratory failure, memory impairment and serious injuries from falls.
This analysis demonstrated that hypnotic use was associated with increased mortality only for the first two years for all classes of drugs; at that point, higher mortality risk was limited to COPD patients who were prescribed benzodiazepines and nonbenzodiazepine benzodiazepine-receptor agonists in comparison to other hypnotics. The authors pointed out that their decision to restrict patients with opiate prescriptions from being included into the database helped minimize bias and confounding.
They said they cannot exclude the possibility, however, that hypnotics were prescribed for amnesic and anxiolytic effects in COPD patients who suffered debilitating diseases shortly before death.
Until more data is available, the study recommended against the long-term use of BZRA hypnotics in COPD patients, instead suggesting that the use of trazodone, orexin receptor antagonists, doxepin Eor melatonin-based medications “may represent a more desirable approach for the treatment of insomnia in COPD patients should the response to behavioral therapy be incomplete or ineffective.”
- El-Solh AA, Lawson Y, Wilding GE. Association Between Hypnotic Use and All-Cause Mortality in Patients with Chronic Obstructive Pulmonary Disease and Insomnia. Int J Chron Obstruct Pulmon Dis. 2023 Nov 3;18:2393-2404. doi: 10.2147/COPD.S430609. PMID: 37942297; PMCID: PMC10629458.
