Rapid Move to Telehealth Helped but Didn’t Stem Participation Losses
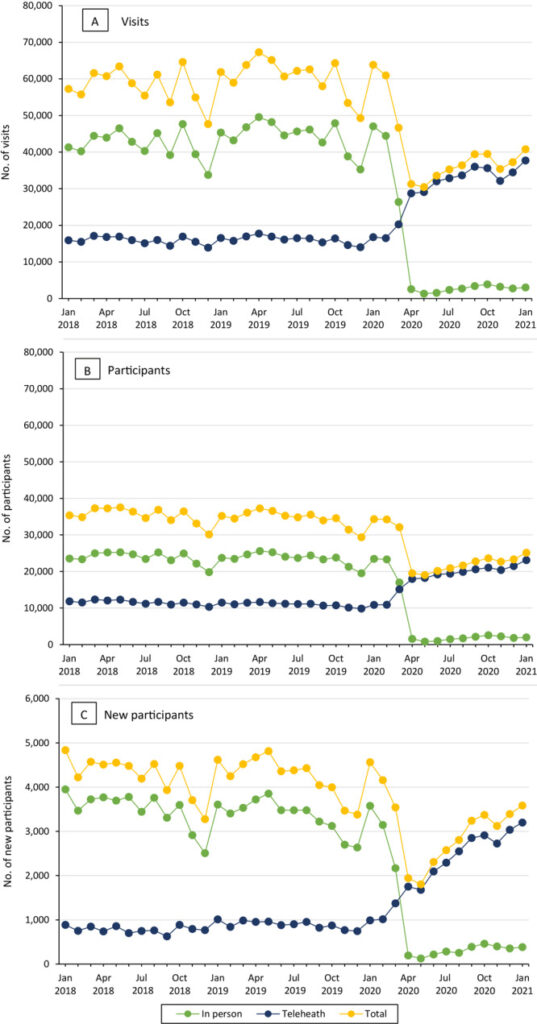
Click To Enlarge: Trends in national Veterans Health Administration MOVE! Weight Management Program participation by modality, January 2018 through January 2021. A, Number of MOVE! visits. B, Number of MOVE! participants. C, Number of new MOVE! participants. Note that the scale in C differs from the scale in A and B. Source: Prev Chronic Dis. 2022; 19: E11.
SEATTLE — The VHA acted quickly to convert its MOVE! Weight Management Program for Veterans to virtual care using telehealth when the COVID-19 pandemic hit in early 2020. But, as expected, participation sharply dropped from previous years—a serious setback for what has been a successful program to combat obesity in veterans.
Most participation in MOVE! was in person before the coronavirus outbreak, according to a recent study, although some telehealth modalities were available. Researchers from the Puget Sound VA Healthcare System and the University of Washington, both in Seattle, sought to describe national trends in MOVE! participation during the pandemic (March 2020-January 2021) overall and by modality and to compare participation to prepandemic levels.
For the study published in the journal Preventing Chronic Disease, the study team conducted a national retrospective cohort study of veterans who participated in MOVE! from January 2018 through January 2021.1
Among the data gathered nationally was the number of visits and participants, as well as new participants in person and via telehealth, including telephone, clinic-to-clinic synchronous video, anywhere-to-anywhere (e.g., provider home to patient home) synchronous video and remote education and monitoring.
Researchers found that, before March 2020, 20% to 30% of MOVE! was delivered via telehealth, but that percentage shot up to 90% by April 2020.
“Early in the pandemic, telephone-delivered MOVE! was the most common modality, but anywhere-to-anywhere synchronous video participation increased over time,” the authors wrote. “Compared with the same months in prior years, total monthly MOVE! participation remained 20% to 40% lower at the end of 2020 and into January 2021.”
They concluded that the VHA MOVE! program “rapidly shifted to telehealth delivery of weight management services in response to the pandemic. However, a gap remained in the number of veterans receiving these services compared with prior years, suggesting potential unmet needs for weight management.”
With 695,050 MOVE! Visits documented in 2018 and 727,585 visits in 2019, that number dropped to 489,939 visits in 2020. “The monthly number of MOVE! visits began to decline sharply in March 2020 because of declines in in-person visits to a nadir in May 2020 of 30,436 visits across modalities,” the study noted.
The nadir of new participants, which dropped precipitously in 2020 compared to the two previous years, was in May 2020, when only 1,803 new patients began MOVE! in that month compared with 4,813 in May 2019.
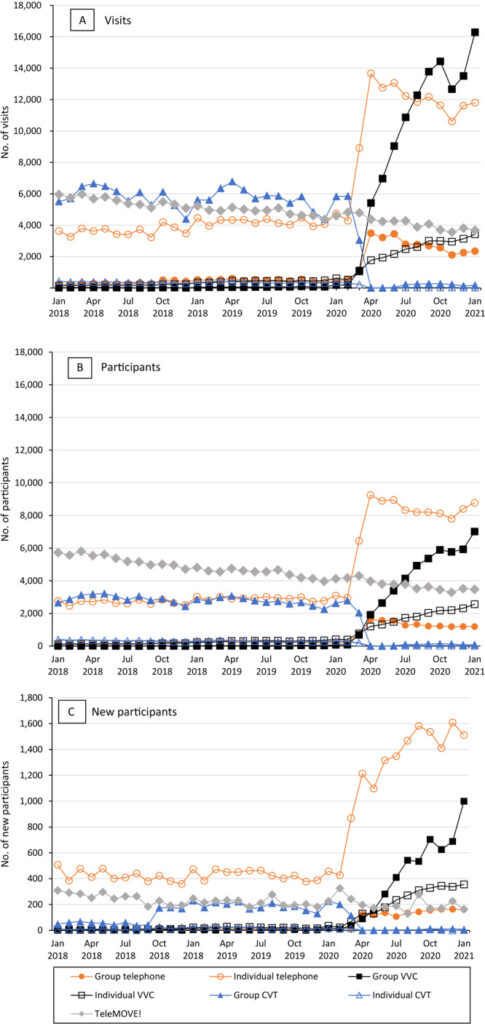
Click To Enlarge: Trends in national Veterans Health Administration telehealth MOVE! Weight Management Program participation by format (group vs individual) and modality, January 2018 through January 2021. A, Number of MOVE! visits. B, Number of MOVE! participants. C, Number of new MOVE! participants. Note that the scale in C differs from the scale in A and B. Abbreviations: VVC, VHA Video Connect; CVT, Clinical Video Telehealth. Source: Prev Chronic Dis. 2022; 19: E11.
Researchers called the declines “dramatic,” explaining that they were partly fueled by “general national VHA guidance in mid-March 2020 to convert appropriate outpatient appointments to virtual modalities and subsequent MOVE!-specific national guidance to suspend in-person MOVE! visits for at least 30 days.”
MOVE! has been offered by the VHA since 2006, to help the more than 80% of veteran patients who have a body mass index (BMI) of 25 or more. The program is an evidence-based comprehensive lifestyle intervention combining dietary, physical activity and behavioral strategies to achieve weight loss of greater than 5%.
MOVE! has been proven effective, resulting in weight loss of 5% or more among 20% to 25% of participants at 12 months. Studies also have found that telehealth individual modalities are as effective as in-person group options, although, before the pandemic, most MOVE! participants attended in-person group sessions at local VHA facilities.
“Given that higher BMI is associated with increased risk of severe COVID-19 among veterans with a BMI of 30 or more, understanding the effect of the pandemic on weight management is critical for anticipating future behavioral weight management needs,” the authors advised. “This knowledge will help the VHA and other health care systems better understand how to address future local or national disruptions in care.”
60% Drop
They reported that, compared with the same month in prior years, total monthly MOVE! participation—in person and telehealth—was 50% to 60% lower in April and May 2020. After May 2020, deficits relative to prior years generally became smaller over time, such as approximately 40% lower in July and August 2020. “However, MOVE! participation remained 20% to 30% lower in the latter months of 2020 and into January of 2021 compared with the same months in prior years,” the authors wrote.
The study noted that the increase in VHA Video Connect participation as the pandemic progressed was related to efforts to educate providers and patients on the newer technology as well as infrastructure improvements to increase bandwidth available for video appointments. That utilization of telephone visits was so high, especially early in the pandemic, was explained by initial national guidance to use the modality with the lowest technology requirement—such as secure messaging or telephone—unless video visits had been established for MOVE! or a veteran requested one.
On the other hand, home telehealth, called TeleMOVE!, essentially remained relatively stable over the pandemic because of new COVID-19 home telehealth monitoring protocols that were developed and guidance to facilities to consider COVID-19 monitoring needs before enrolling new TeleMOVE! participants.
When MOVE! staff was reassigned to provide COVID-19 care, remaining teams were urged to prioritize telehealth options based on patient needs and characteristic.
The resulting declines in use were stark, according to researchers, who explained that “many patients who would have otherwise received weight management services did not because of the pandemic. Given COVID-19–related declines in physical activity, increases in sedentary behaviors, and changes in eating patterns, there is a pressing need for accessible weight management services now and in the future.”
The problem goes beyond inability to attend MOVE! meetings in person, they added. “Contributors to changes in health behaviors may include COVID-19 restrictions leading to shifts in routine or access to healthy foods and safe spaces for physical activity (eg, lack of access to gyms or exercise partners). Psychological distress also increased markedly during the pandemic, which may be a factor in worsening activity and eating behaviors, given that conditions such as depression and posttraumatic stress disorder affect health behaviors and weight.”
The authors pointed out that patients might have coped with distress by eating comfort foods or had to focus on virtual schooling of children instead of focusing on weight management. “Related to these and other factors, 42% of U.S. adults reported gaining unwanted weight during the pandemic, with an average gain of 29 pounds. With high rates of mental health conditions, food insecurity, and limited social support, veterans may be especially vulnerable to COVID-19-related behavior change and weight gain.”
The study team suggested that MOVE! might need to take on additional strategies to help mitigate heightened pandemic-related stress and anxiety.
“Our findings also suggest that barriers to telehealth may remain at the patient, provider, or health care system level,” the authors wrote. “One such potential barrier is the lack of technology necessary for telehealth weight management services.”
As to how MOVE! participants might have perceived telehealth during COVID-19 restrictions, a 2021 survey among 58 veterans who were seen during the pandemic in an intensive weight management clinic that provides interdisciplinary pre- and postbariatric surgery care might offer some insights, according to study authors. Half of the participants said they found telephone visits as good as in-person visits, and about the same percentage said they would prefer to have all visits over the telephone even without pandemic-related restrictions.4
While the participants were not offered video visits, they were asked about preference for that modality. About half indicated they would have preferred video to telephone visits if they were available, and 37% said they would prefer all video visits even after restrictions were lifted.
Yet, many veterans lack the technology required for video visits, including compatible devices or high-speed internet, according to authors of the more recent study. “These barriers differentially affect older, unhoused, and rural veterans,” they wrote, advising that the VHA tried to address the gaps by implementing the Digital Divide Consult. The program enables patients to obtain internet services or technology needed for VHA telehealth.
“However, the VHA will need to evaluate the extent to which the pandemic exacerbated disparities in access and the success of the Digital Divide Consult in addressing these disparities,” the study emphasized. “Given anticipated long-term shifts toward reliance on telehealth, the VHA must continue to ensure equitable access for all veterans.”
The authors also raised the possibility that finding a way to bring back face-to-face weight-management programs, including group programs, might be possible. They suggested that those could include se of face masks, social distancing, proper ventilation, hand hygiene and encouraging vaccination and boosters.
Other possibilities might be “offering hybrid models with in-person and telehealth options; continuing to provide MOVE! via synchronous video and telephone; and expanding self-directed options, like app, online, or DVD-based programs, which have been effective in non-VHA settings and are currently being tested in the VHA.”
The generally positive acceptance of telehealth for weight loss might be important for the future, the researchers pointed out, explaining that “demand for weight management services may increase in the postpandemic recovery period, which could be met by health care systems offering telehealth or hybrid options.”
- Gray KE, Hoerster KD, Spohr SA, Breland JY, Raffa SD. National Veterans Health Administration MOVE! Weight Management Program Participation During the COVID-19 Pandemic. Prev Chronic Dis. 2022 Mar 10;19:E11. doi: 10.5888/pcd19.210303. PMID: 35271436; PMCID: PMC893762
- Maciejewski ML, Shepherd-Banigan M, Raffa SD, Weidenbacher HJ. Systematic Review of Behavioral Weight Management Program MOVE! for Veterans. Am J Prev Med. 2018 May;54(5):704-714. doi: 10.1016/j.amepre.2018.01.029. Epub 2018 Mar 15. PMID: 29550164.
- Rutledge T, Skoyen JA, Wiese JA, Ober KM, Woods GN. A comparison of MOVE! versus TeleMOVE programs for weight loss in Veterans with obesity. Obes Res Clin Pract. 2017 May-Jun;11(3):344-351. doi: 10.1016/j.orcp.2016.11.005. Epub 2016 Dec 5. PMID: 27931766.
- Lohnberg JA, Salcido L, Frayne S, Mahtani N, Bates C, Hauser ME, Breland JY. Rapid conversion to virtual obesity care in COVID-19: Impact on patient care, interdisciplinary collaboration, and training. Obes Sci Pract. 2021 Aug 28;8(1):131–6. doi: 10.1002/osp4.550. Epub ahead of print. PMID: 34540265; PMCID: PMC8441727
