VA Faces Growing Problem of Frailty Among Aging Patients
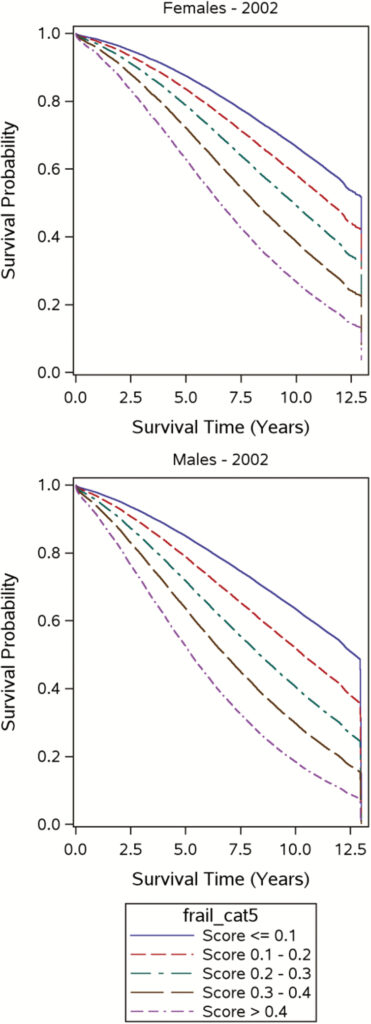
Click to Enlarge: Kaplan–Meier curves for mortality in men and women (2002–2014). Source: The Journals of Gerontology Series A
MIAMI — Older veterans diagnosed with frailty are at much greater risk of developing long COVID after acute infection with SARS-CoV-2, according to a new study. Making that especially significant is that so many older VHA patients, including those living in the community, meet the criteria for frailty.
“Older populations have suffered the highest rates of SARS-CoV-2 infection and associated complications, including Post-Acute Sequelae of SARS-CoV-2 infection (PASC),” according to a new study in the Journal of the American Geriatric Society. “Frailty is a geriatric syndrome that often coexists with COVID-19 infection. The vulnerability to stressors caused by multisystemic dysfunction that characterizes frailty may predispose older adults to develop PASC.”1
A team led by researchers from the Miami VA Healthcare System and the University of Miami Miller School of Medicine conducted a retrospective cohort study using the VA COVID-19 Shared Data Resource. The goal was to identify US veterans testing positive for SARS-CoV-2 between July 2021 and February 2022, without prior positive tests and who were alive 30 days after infection.
At the same time, frailty was calculated using a 31-item VA Frailty Index with information gathered from electronic health records. The researchers categorized Veterans into robust (FI ≤ 0.10), prefrail (FI: >0.10- < 0.21), and frail (FI ≥ 0.21). They assessed the association between frailty and PASC, also called Long COVID, and vaccination and PASC, adjusting for covariates.
The frailty index included the following health domains:
- morbidity (e.g., diabetes, kidney disease),
- functional status (e.g., arthritis, use of durable medical equipment and resources [e.g., motorized wheelchair,
- home-based practitioner care]),
- cognition and
- mood (e.g., dementia, depression),
- sensory loss (e.g., blindness, hearing impairment), and
- other conditions common among older adults (e.g., chronic pain, weight loss in past year).
The study identified 245,857 COVID-19-positive veterans surviving 30 days after infection. Their mean age was 57.5± 16.5 years; 87.2% were males, 68.1% were white, and 9.0% were Hispanic. Nearly half of the sample (48.9%) were classified as robust, while 28.3% were pre-frail, and 22.7% were frail. Of the total, 99,886 (40.6%) were fully vaccinated, and 33,516 (13.6%) received booster doses.
Results indicated that, over a median follow-up of 143 days (IQR = 101), 23,890 (9.7%) patients developed PASC. “Within 6 months after infection, frailty and pre-frailty were associated with a 41% (adjusted HR [aHR]:1.40 (95% CI: 1.35-1.47)) and 15% (aHR: 1.17 (95% CI: 1.11-1.19)) increase in the risk of PASC compared with the robust, respectively,” the authors wrote.”Vaccination and booster doses before infection were associated with a 27% (aHR: 0.73 (95% CI: 0.71-0.75)) and 33% (aHR: 0.66 (95% CI: 0.63-0.69)) reduction in the risk of developing PASC, respectively”.
The researchers concluded that frailty was associated with an increased risk of developing PASC, while vaccination was associated with a decreased risk of PASC, which was further reduced by booster doses.
“Early recognition of frailty in patients with COVID-19 may assist in the early identification and management of PASC,” they advised.
A 2020 study, also from the Miami VA Healthcare System, showed a high incidence of frailty in community dwelling older U.S. veterans.
Community-Dwelling
The article in the Journal of the American Medical Directors Association reported the results of a population-based retrospective cohort study including community-dwelling veterans 60 years and older. Participants had a determination of frailty from 2013 to 2014 and were followed until September 2019.
The study team generated a 31-item frailty index at baseline and during each subsequent primary care encounters, using electronic health record data, for 15,761 veteran patients. The cohort had a mean age 72.18 (9.32) years with 74% Caucasian, 90.75% non-Hispanic and 97.78% male.
“The period prevalence of frailty in this cohort was 20.84%,” the researchers reported. “Over a median follow-up of 3.96 (interquartile range = 3.73) years, 25.86% of the baseline population died during follow up. Veterans with frailty had a higher all-cause mortality during follow up, adjusted hazard ratio = 3.12 (95% confidence interval 2.87-3.38), P value of < .0005.”
The study pointed out that, among 10,513 veterans who survived a median follow-up of 4.81 (interquartile range = 3.12) years, 29.84% became frail. The incidence rate of frailty was 75.05 cases per 1,000 person-years. In addition, among the entire cohort of 13,268 nonfrail veterans, 29.93% became frail. The incidence rate of frailty for the veterans was 84.03 cases per 1000 person-years.
“Future studies should be done for identification, implementation of adequate interventions aimed at preventing frailty or reducing frailty-related complications in community dwelling older individuals,” the researchers advised.
A 2019 study found that frailty affects at least 3 of every 10 U.S. veterans aged 65 years and older, and is strongly associated with mortality.3
“The accelerated pace of population aging presents a formidable challenge to health care systems worldwide,” wrote VA Boston Healthcare System researchers and colleagues. “This is especially true for the Department of Veterans Affairs (VA), as over 4.5 million U.S. Veterans are now 75 and older, creating an urgent need to promote healthier aging and target resources to those who need them most.”
- Hammel IS, Tosi DM, Tang F, Pott H, Ruiz JG. Frailty as a risk factor for post-acute sequelae of COVID-19 among US veterans during the Delta and Omicron waves. J Am Geriatr Soc. 2023 Sep 19. doi: 10.1111/jgs.18584. Epub ahead of print. PMID: 37725480.
- Ganta N, Sikandar S, Ruiz SJ, Nasr LA, Incidence of Frailty in Community-Dwelling United States Older Veterans. J Am Med Dir Assoc. 2021 Mar;22(3):564-569. doi: 10.1016/j.jamda.2020.10.019. Epub 2020 Nov 15. PMID: 33234447.
- Orkaby AR, Nussbaum L, Ho YL, Gagnon D, et. al. The Burden of Frailty Among U.S. Veterans and Its Association With Mortality, 2002-2012. J Gerontol A Biol Sci Med Sci. 2019 Jul 12;74(8):1257-1264. doi: 10.1093/gerona/gly232. PMID: 30307533; PMCID: PMC6625596.
