Click to Enlarge: Age was determined in March 2022, when the US Food and Drug Administration authorized a second booster vaccination for persons 50 years or older. Source: Jama Network Open
PORTLAND, OR — Public health officials can better target their message if they better understand where COVID-19 primary and booster vaccine uptake is low. A new VA study suggests that whether the potential recipient lives in a rural or urban area can be an important factor.
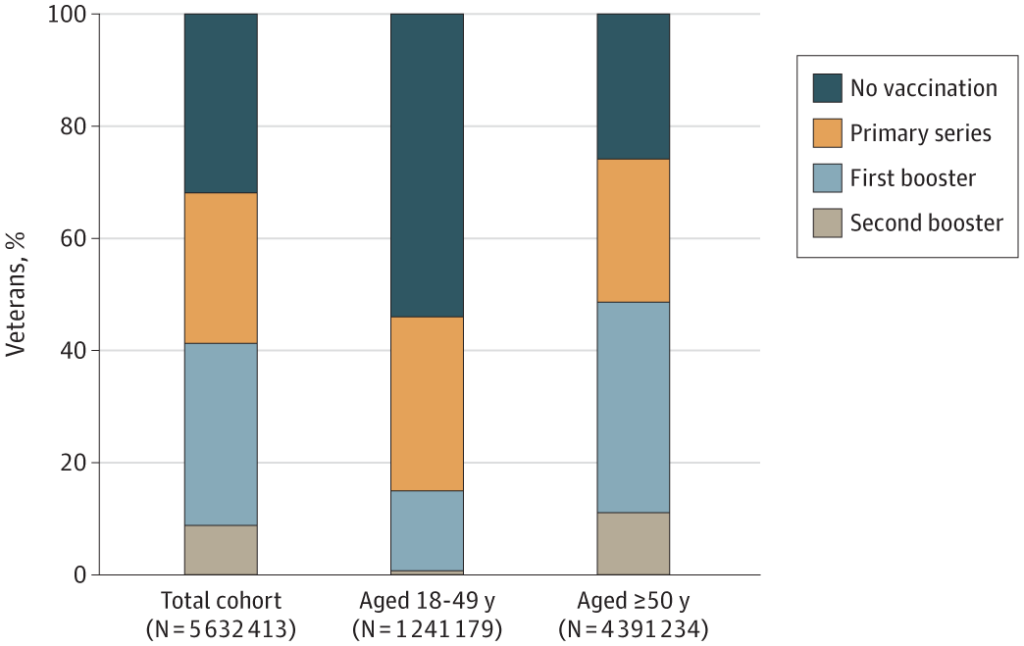
The research focused on COVID-19 primary and booster vaccinations at the VHA from December 2020 to June 2022. The cohort study of nearly 6 million enrolled veterans finds that 69.0% received a primary vaccination, 42.9% a first booster and a substantially lower 9.3% for the second booster.
The report in JAMA Network Open advises that older age, Asian or Black race, Hispanic ethnicity and urban residence were independently associated with getting the vaccines. On the other hand, according to the study led by the Veterans Affairs Portland Health Care System and the Oregon Health and Science University in Portland, younger, rural veterans might require more targeting.1
“COVID-19 vaccination rates remain suboptimal in the U.S. Identifying factors associated with vaccination can highlight existing gaps and guide targeted interventions to improve vaccination access and uptake,” the authors point out.
The researchers set out to describe the incidence and patient characteristics associated with primary, first booster, and second booster COVID-19 vaccination in the Veterans Health Administration (VHA).
Among the veterans included in the study, more than 90% were male, with a median age of 66. Of those, 18.3% were Black, 8% Hispanic and 74.6% were white.
“Cumulative incidence for primary vaccination increased with increasing age, from 46.9% (95% CI, 46.8%-47.0%) among veterans aged 18 to 49 years to 82.9% (95% CI, 82.8%-83.0%) among veterans aged 80 to 84 years,” according to the study. “More Black veterans completed primary vaccination (71.7%; 95% CI, 71.6%-71.8%) compared with white veterans (68.9%; 95% CI, 68.9%-69.0%), and more urban-dwelling veterans completed primary vaccination (70.9%; 95% CI, 70.9%-71.0%) compared with highly rural-dwelling veterans (63.8%; 95% CI, 63.4%-64.1%).”
Researchers noted that factors independently associated with a higher likelihood of both primary and booster vaccination included older age, female sex, Asian or Black race, Hispanic ethnicity, urban residence and lack of prior SARS-CoV-2 infection.
“In this cohort study of U.S. veterans, COVID-19 vaccination coverage through June 2022 was suboptimal. Primary vaccination can be improved among younger, rural-dwelling veterans,” the study concludes. “Greater uptake of booster vaccination among all veterans is needed.”
The authors added that few studies “have comprehensively described sociodemographic, geographic, and clinical factors associated with receipt of primary and booster vaccination.”
They pointed out, “As observed in the general U.S. population, compared with older veterans, we found that uptake of vaccination among younger veterans has remained lower. More than half (54.0%) of veterans in care aged 18 to 49 years were unvaccinated, whereas 31.1% had completed primary vaccination only.”
The study authors wrote that even veterans aged 50 to 69 years had significantly lower vaccine receipt than in older groups. “Differences in risk perception of SARS-CoV-2 infection and related outcomes, vaccine safety and efficacy, and trust in authorities may contribute to a lower incidence and likelihood of vaccination among younger groups,” the researchers suggested.
- Bajema KL, Rowneki M, Berry K, et al. Rates of and Factors Associated With Primary and Booster COVID-19 Vaccine Receipt by US Veterans, December 2020 to June 2022. JAMA Netw Open. 2023;6(2):e2254387. doi:10.1001/jamanetworkopen.2022.54387
