Even Healthy Veterans With Mild Cases Were at Higher Risk
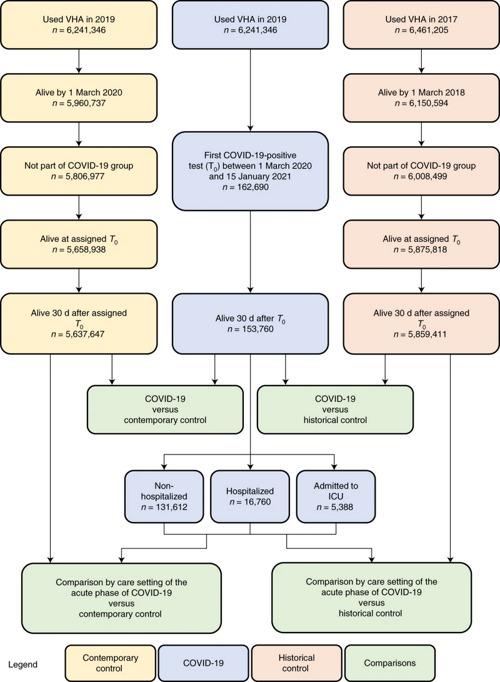
Click to Enlarge: Cohort construction for COVID-19 group (blue), contemporary control group (yellow) and historical control group (orange). Comparisons between groups are presented in green. Nature Medicine (Nat Med)
ST. LOUIS — When it comes to cardiovascular complications, the acute care of COVID-19 symptoms in veterans appears to be only the first stage for what, in some cases, turns out to be a longer-term healthcare crisis.
A VA study published in Nature Medicine found that patients recovered from infection with SARS-CoV-2 are at much higher risk of developing cardiovascular issues within the first month to a year after infection. Those include disruptive heart rhythms, inflammation of the heart, blood clots, stroke, coronary artery disease, heart attack, heart failure or even death.1
Even more disturbing, according to researchers from the VA St. Louis Healthcare System and Washington University School of Medicine, those cardiovascular complications are occurring in patients who were healthy prior to COVID-19 and who, in some cases, had only mild cases.
“We wanted to build upon our past research on COVID’s long-term effects by taking a closer look at what’s happening in people’s hearts,” said senior author Ziyad Al-Aly, MD, of the St. Louis VAMC. assistant professor of medicine at Washington University. “What we’re seeing isn’t good. COVID-19 can lead to serious cardiovascular complications and death. The heart does not regenerate or easily mend after heart damage. These are diseases that will affect people for a lifetime.”
More than 380 million people globally have been infected with the virus since the pandemic started, according to the study report.
“Consequently, COVID-19 infections have, thus far, contributed to 15 million new cases of heart disease worldwide,” added Al-Aly, who also is an assistant professor at Washington University School of Medicine. “This is quite significant. For anyone who has had an infection, it is essential that heart health be an integral part of post-acute COVID care.”
The study pointed out that, while the cardiovascular complications of acute coronavirus disease 2019 (COVID-19) are well known and have been extensively detailed, much less is known about the post-acute cardiovascular manifestations of COVID-19. To remedy that, the research team used the VA’s national healthcare databases to build a cohort of 153,760 COVID-19 patients as well as two sets of control cohorts with 5,637,647 (contemporary controls) and 5,859,411 (historical controls) veterans to estimate risks and one-year burdens of a set of prespecified incident cardiovascular outcomes.
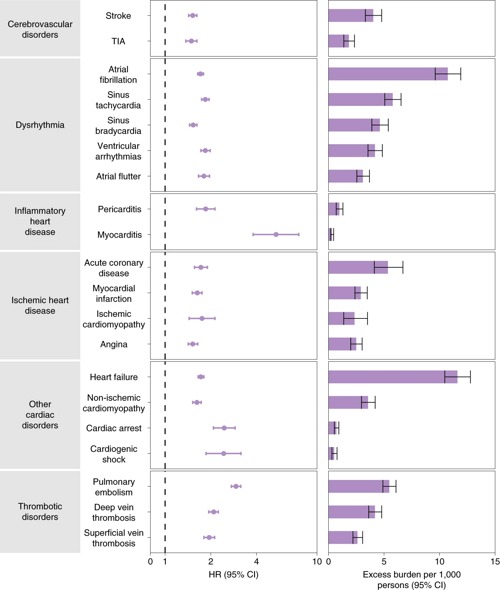
Click to Enlarge: Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 153,760) and contemporary control cohort (n = 5,637,647). Adjusted HRs and 95% CIs are presented. The length of the bar represents the excess burden per 1,000 persons at 12 months, and associated 95% CIs are also shown. Nature Medicine (Nat Med)
“We show that, beyond the first 30 days after infection, individuals with COVID-19 are at increased risk of incident cardiovascular disease spanning several categories, including cerebrovascular disorders, dysrhythmias, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure and thromboembolic disease,” the authors advised. “These risks and burdens were evident even among individuals who were not hospitalized during the acute phase of the infection and increased in a graded fashion according to the care setting during the acute phase (non-hospitalized, hospitalized and admitted to intensive care).”
The study found that patients who survived the first 30 days of COVID-19 exhibited increased risk of stroke (hazard ratio (HR) = 1.52 (1.43, 1.62); burden 4.03 (3.32, 4.79) per 10,00 persons at 12 months; for all HRs and burdens, parenthetical ranges refer to 95% confidence intervals (CIs)) and transient ischemic attacks (TIA) (HR = 1.49 (1.37, 1.62); burden 1.84 (1.38, 2.34)). The risks and burdens of a composite of these cerebrovascular outcomes were 1.53 (1.45, 1.61) and 5.48 (4.65, 6.35).
The report discussed several cardiovascular subcategories, including increased risks of:
Dysrhythmias
Atrial fibrillation (HR = 1.71 (1.64, 1.79); burden 10.74 (9.61, 11.91)), sinus tachycardia (HR = 1.84 (1.74, 1.95); burden 5.78 (5.07, 6.53)), sinus bradycardia (HR = 1.53 (1.45, 1.62); burden 4.62 (3.90, 5.38)), ventricular arrhythmias (HR = 1.84 (1.72, 1.98); burden 4.18 (3.56, 4.85)); and atrial flutter (HR = 1.80 (1.66, 1.96); burden 3.10 (2.55, 3.69)). The risks and burdens of a composite of these dysrhythmia outcomes were 1.69 (1.64, 1.75), and 19.86 (18.31, 21.46).
Inflammatory Disease of the Heart or Pericardium
Inflammatory disease of the heart or pericardium included pericarditis (HR = 1.85 (1.61, 2.13)); burden 0.98 (0.70, 1.30) and myocarditis (HR = 5.38 (3.80, 7.59); burden 0.31 (0.20, 0.46)). The risks and burdens of a composite of these inflammatory diseases of the heart or pericardium were 2.02 (1.77, 2.30) and 1.23 (0.93, 1.57).
Ischemic Heart Disease
Ischemic heart disease including acute coronary disease (HR = 1.72 (1.56, 1.90); burden 5.35 (4.13, 6.70)), myocardial infarction (HR = 1.63 (1.51, 1.75); burden 2.91 (2.38, 3.49)), ischemic cardiomyopathy (HR = 1.75 (1.44, 2.13); burden 2.34 (1.37, 3.51)) and angina (HR = 1.52 (1.42, 1.64); burden 2.50 (2.00, 3.03)). The risks and burdens of a composite of these ischemic heart disease outcomes were 1.66 (1.52, 1.80) and 7.28 (5.80, 8.88).
Other Cardiovascular Disorders
Other cardiovascular disorders included heart failure (HR = 1.72 (1.65, 1.80); burden 11.61 (10.47, 12.78)), nonischemic cardiomyopathy (HR = 1.62 (1.52, 1.73); burden 3.56 (2.97, 4.20)), cardiac arrest (HR = 2.45 (2.08, 2.89); burden 0.71 (0.53, 0.93)) and cardiogenic shock (HR = 2.43 (1.86, 3.16); burden 0.51 (0.31, 0.77)). The risks and burdens of a composite of these other cardiovascular disorders were 1.72 (1.65, 1.79) and 12.72 (11.54, 13.96).
Thromboembolic Disorders
Thromboembolic disorders included pulmonary embolism (HR = 2.93 (2.73, 3.15); burden 5.47 (4.90, 6.08)); deep vein thrombosis (HR = 2.09 (1.94, 2.24); burden 4.18 (3.62, 4.79)) and superficial vein thrombosis (HR = 1.95 (1.80, 2.12); burden 2.61 (2.20, 3.07)). The risks and burdens of a composite of these thromboembolic disorders were 2.39 (2.27, 2.51) and 9.88 (9.05, 10.74).
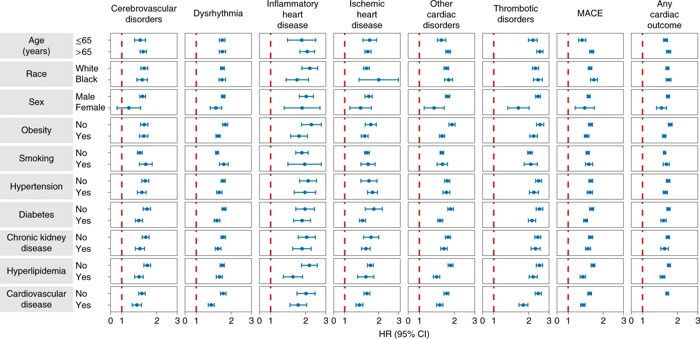
Click to Enlarge: Composite outcomes consisted of cerebrovascular disorders (stroke and TIA), dysrhythmias (atrial fibrillation, sinus tachycardia, sinus bradycardia, ventricular arrhythmias and atrial flutter), inflammatory heart disease (pericarditis and myocarditis), ischemic heart disease (acute coronary disease, myocardial infarction, ischemic cardiomyopathy and angina), other cardiac disorders (heart failure, non-ischemic cardiomyopathy, cardiac arrest and cardiogenic shock), thrombotic disorders (pulmonary embolism, deep vein thrombosis and superficial vein thrombosis), MACE (all-cause mortality, stroke and myocardial infarction) and any cardiovascular outcome (incident occurrence of any cardiovascular outcome studied). Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 153,760) and contemporary control cohort (n = 5,637,647). Adjusted HRs and 95% CIs are presented. Nature Medicine (Nat Med)
Researchers also looked at the risks and burdens of two composite endpoints, including major adverse cardiovascular event (MACE) — a composite of myocardial infarction, stroke and all-cause mortality—and any cardiovascular outcome (defined as the occurrence of any incident prespecified cardiovascular outcome included in this study). Compared to the contemporary control group, they found increased risks and burdens of MACE (HR = 1.55 (1.50, 1.60); burden 23.48 (21.54, 25.48)) and any cardiovascular outcome (HR = 1.63 (1.59, 1.68); burden 45.29 (42.22, 48.45)).
The risks of incident composite cardiovascular outcomes also were analyzed in subgroups based on age, race, sex, obesity, smoking, hypertension, diabetes, chronic kidney disease, hyperlipidemia and cardiovascular disease. The study team determined that the risks of incident composite cardiovascular outcomes were evident in all subgroups.
Because of the evidence that the risk and one-year burden of cardiovascular disease in survivors of acute COVID-19 are outsized, researchers recommended that care pathways of those surviving the acute episode of COVID-19 should include attention to cardiovascular health and disease.
The findings provide strong evidence that cardiovascular complications can occur regardless of age, race, sex or other risk factors, including obesity, hypertension, diabetes, chronic kidney disease and hyperlipidemia. The authors emphasize that the heart manifestation were found in patients without any cardiovascular disease before exposure to COVID-19, “providing evidence that these risks might manifest even in people at low risk of cardiovascular disease.”
Researchers pointed to two key finding that the risks and associated burdens:
- Were evident among those who were not hospitalized during the acute phase of the disease—this group represents the majority of people with COVID-19; and
- Exhibited a graded increase across the severity spectrum of the acute phase of COVID-19 from nonhospitalized to hospitalized individuals to those admitted to intensive care.
“Taken together, our results show that 1-year risks and burdens of cardiovascular diseases among those who survive the acute phase of COVID-19 are substantial and span several cardiovascular disorders,” the authors wrote. “Care strategies of people who survived the acute episode of COVID-19 should include attention to cardiovascular health and disease.”

