A Half of a Million SARS-CoV-2 Survivors Might Have Those Issues
ST. LOUIS — Patients who recover from COVID-19 often suffer long-term consequences. One of the most dangerous, according to a new veterans’ study, is the detrimental effects on kidney function, which might affect hundreds of thousands of survivors.
So-called long COVID is often seen in terms of pulmonary effects, but extrapulmonary organ systems also can be involved.
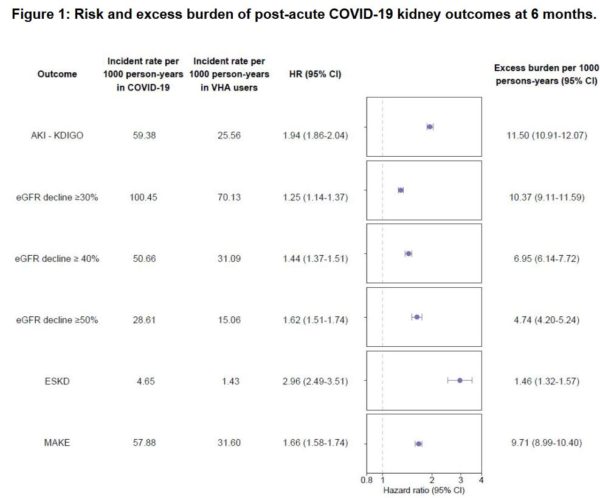
The report in the Journal of the American Society of Nephrology noted that “beyond the acute phase of illness, 30-day survivors of COVID-19 exhibited higher risks of AKI, eGFR decline, ESKD, major adverse kidney events (MAKE), as well as steeper longitudinal decline in eGFR.” Researchers from the VA St. Louis Healthcare System and Washington University School of medicine, both in Missouri, pointed out that the risks of kidney outcomes increased in line with the severity of the acute infection (i.e., whether the patient was nonhospitalized, hospitalized or admitted to intensive care).1
“Our findings emphasize the critical importance of paying attention to kidney function and disease in caring for patients who have had COVID-19,” said senior author Ziyad Al-Aly, MD. “If kidney care isn’t an integral part of COVID-19 post-acute care strategy, then we will miss opportunities to help potentially hundreds of thousands of people who have no idea that their kidney function has declined due to this virus. This is in addition to the millions of Americans who suffer from kidney disease not caused by COVID-19.”
Based on the research, Al-Aly suggested that more than a half-million patients who recovered from COVID-19 might have kidney injury or disease.
For the study, researchers created a cohort of 1.7 million veterans identified from March 1, 2020, to March 15, 2021; that included 89,216 30-day COVID-19 survivors and about 1.6 million noninfected controls. The team looked at risks of acute kidney injury, eGFR decline, end-stage kidney disease and major adverse kidney events (MAKEMAKE, which is defined as eGFR decline ≥50%, ESKD, or all-cause mortality.
Results indicated that, even past acute illness, 30-day survivors of COVID-19 exhibited a higher risk of AKI (aHR=1.94 (95%CI: 1.86,2.04)), eGFR decline ≥30% (1.25 (1.14,1.37)), eGFR decline ≥40% (1.44 (1.37,1.51)), eGFR decline ≥50% (1.62 (1.51,1.74)), ESKD (2.96 (2.49-3.51)), and MAKE (1.66 (1.58,1.74)).
“There was a graded increase in risks of post-acute kidney outcomes according to the severity of the acute infection (whether patients were non-hospitalized, hospitalized, or admitted to intensive care,” researchers explained.
The authors advised that, compared to noninfected controls, 30-day COVID-19 survivors exhibited excess eGFR decline of -3.26 (-3.58, -2.94), -5.20 (-6.24, -4.16) and -7.69 (-8.27, -7.12) mL/min/1.73m2/year in nonhospitalized, hospitalized and those admitted to intensive care during the acute phase of COVID-19 infection.
Most of the COVID-19 patients in the study were male and in their late 60s. Researchers also analyzed data, however, that included 151,289 women—including 8,817 with COVID-19—and adults of all ages. They reported that, among the COVID-19 patients, 12,376 (13.9%) required hospitalization, including 4,146 (4.6%) who were admitted to intensive care units (ICUs).
ICU Patients Most Affected
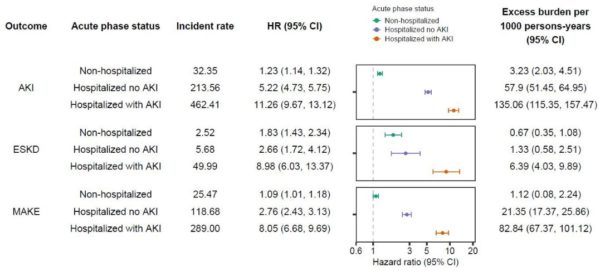
Click To Enlarge: Risk and excess burden of post-acute COVID-19 kidney outcomes at 6 months in mutually exclusive cohorts of Veterans with non-hospitalized COVID-19, hospitalized COVID-19 with no evidence of an AKI, and those hospitalized with COVID-19 with an AKI during the first 30 days (acute phase) of the infection.
“The risk of decreased kidney function is highest among people who were in the ICU; however, it’s important to note that the risk extends to all patients, even those who had milder cases of COVID-19,” said Al-Aly, who also is director of the Clinical Epidemiology Center and chief of the Research and Education Service at the Veterans Affairs St. Louis Health Care System.
“It’s essential to discover kidney dysfunction before the problem progresses and becomes harder to treat,” he explained. “But kidney problems are silent problems that won’t be found until somebody checks the blood work. Based on our research, it’s especially important that healthcare providers do this for people who have had COVID-19. Otherwise, we’ll miss a lot of people and, sadly, we’ll be dealing with more advanced kidney diseases down the road.”
Even patients who didn’t require hospitalization faced a high risk of kidney issues than uninfected veterans. That included:
- 15% higher risk of suffering from a major adverse kidney event such as chronic kidney disease,
- 30% higher risk of developing acute kidney injury, and
- 215% (more than twofold) higher risk of acquiring end-stage kidney disease, where kidneys can no longer effectively remove waste from the body and dialysis or a kidney transplant is required.
It was even worse for patients hospitalized for COVID-19—and much more dangerous for those who required critical care—with seven times the risk of experiencing a major adverse kidney event, eight times the risk of acute kidney injury and 13 times the risk of end-stage kidney disease, the authors reported.
“People who were hospitalized for COVID-19 or needed ICU care are at the highest risk,” Al-Aly said. “But the risk is not zero for those who had milder cases. In fact, it’s significant. And we need to remember that we don’t yet know the health implications for long-haulers in the coming years.”
Patients with milder COVID-19 cases had 1.09 times the risk of having an estimated GFR decline of 30% or more; that went up to double the risk for hospitalized patients not in intensive care units and triple the risk for those who spent time in intensive care.
“The kidney damage was in excess of reduced function caused by normal aging,” Al-Aly pointed out. “A 60-year-old’s kidney function is less robust than the kidneys of a 20-year-old. The kidney function decline we’ve observed in these patients is not graceful aging. It is not normal anything. It is definitely a disease state.
“Kidney disease is one important facet of the multifaceted long COVID-19,” he added. “It is a critical component of the long COVID-19 story, and it must be taken into account when caring for people with long COVID-19.”
Kidney dysfunction and disease are considered to be silent killers, because patients often are free of pain and other symptoms. In fact, the National Kidney Foundation estimates that 90% of kidney disease patients don’t know it. The condition is estimated to affect about 37 million people in the United States and is a leading cause of death.
- Bowe B, Xie Y, Xu E, Al-Aly Z. Kidney Outcomes in Long COVID. J Am Soc Nephrol. 2021 Sep 1:ASN.2021060734. doi: 10.1681/ASN.2021060734. Epub ahead of print. PMID: 34470828.