Click to Enlarge: Adjusted Mean Wait Time by Race and Ethnicity and Time Period Source: Jama Network Open
BOSTON — Black and Hispanic veterans appeared to experience more barriers to accessing care than white veterans during the COVID-19 pandemic, according to a new study finding that wait time disparities increased significantly from the pre–COVID-19 period.
An article published in JAMA Network Open sought to determine whether wait times earlier in the pandemic increased differentially for Black and Hispanic veterans compared with white veterans receiving VHA care. The cross-sectional study included about 1.2 million veterans. The veterans included in the study had a mean age of 63.4 and were 80.8% men.1
“Prior studies indicate that Black and Hispanic vs White veterans wait longer for care,” according to authors from the Center for Health Care Organization and Implementation Research at the VA Boston Healthcare System and colleagues. “However, these studies do not capture the COVID-19 pandemic, which caused care access disruptions, nor implementation of the U.S. Department of Veterans Affairs (VA) Maintaining Internal Systems and Strengthening Integrated Outside Networks Act (MISSION), which is intended to improve care access by increasing veterans’ options to use community clinicians.
Also involved in the study were researchers from the Center for Access & Delivery Research and Evaluation at the VA Iowa City, IA, Health Care System.
The study team sought to determine whether wait times increased differentially from the pre–COVID-19 to COVID-19 periods, in light of the MISSION implementation. Data was obtained from the VA’s Corporate Data Warehouse for fiscal years 2019 to 2021 (Oct. 1, 2018, to Sept. 30, 2021). Specifically, information was gathered on veterans with a new consultation for outpatient cardiology and/or orthopedic services during the study period. The focus was on overall mean wait times and facility-level adjusted relative mean wait time ratios, as well as racial-ethnic difference.
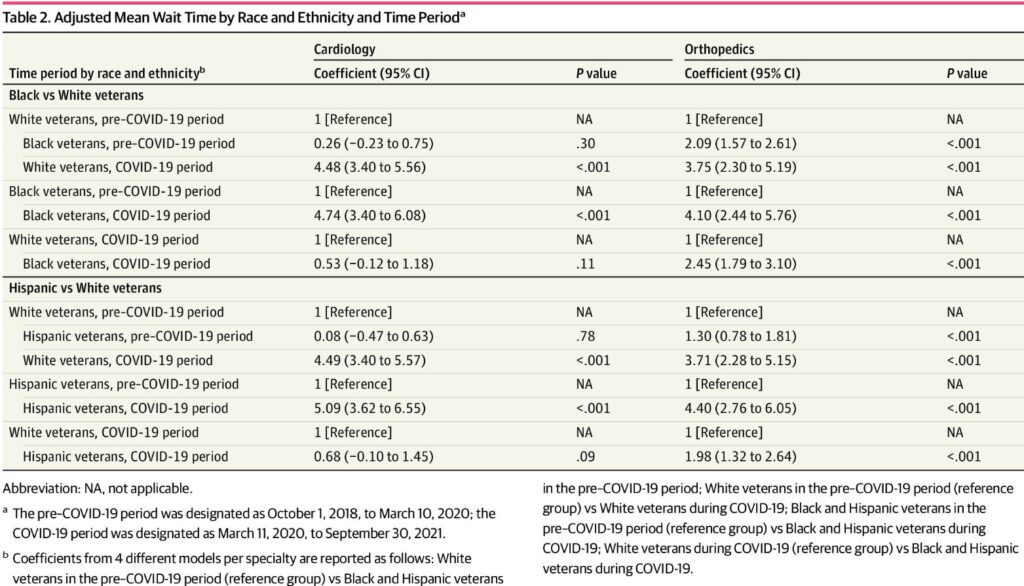
Results indicated that significant wait time disparities occurred for orthopedic services; researchers pointed out that Black veterans had wait times 2.09 [95% CI, 1.57-2.61] days longer than those for white veterans) in the pre-COVID-19 period. Those trends were not seen for cardiology services, however.
“Mean wait times increased from the pre–COVID-19 to COVID-19 periods for both services for all three racial and ethnic groups (e.g., Hispanic wait times for cardiology services increased 5.09 [95% CI, 3.62-6.55] days,” the researchers advised. “Wait time disparities for Black veterans (4.10 [95% CI, 2.44-5.19] days) and Hispanic veterans (4.40 [95% CI, 2.76-6.05] days) vs White veterans (3.75 [95% CI, 2.30-5.19] days) increased significantly from the pre-COVID-19 to COVID-19 periods (P < 0.001). During the COVID-19 period, significant disparities were evident for orthopedic services (e.g., mean wait times for Hispanic vs White veterans were 1.98 [95% CI, 1.32-2.64] days longer) but not for cardiology services.”
The authors added that, while wait time ratios varied across the 140 facilities, only six facility wait time ratios were significant during the pre-COVID-19 period and 26 during the COVID-19 period.
“These findings suggest that wait time disparities increased from the pre–COVID-19 to COVID-19 periods, especially for orthopedic services for both Black and Hispanic veterans, despite MISSION’s goal to improve access,” the study concluded. “Facility-level analyses identified potential sites that could be targeted to reduce disparities.”
Disparate Impact
Background information in the articles advised that delayed and disrupted care can adversely affect morbidity and mortality, while also decreasing healthcare utilization and the quality of patient experience. “For these reasons, wait time (the amount of time it takes a patient to get an appointment and see a clinician) has emerged as a key indicator of overall health system performance,” the authors explained. “It is also why disparities in care access, evident for certain subgroups (e.g., Black and Hispanic adults) are concerning. The disparate impact of the COVID-19 pandemic further brought care access disparities into sharper focus.”
The study recounted how, among a national sample of adults in the United States, an estimated 40.9% reported delayed care or avoided care because of the COVID-19 pandemic, with delayed care significantly higher for Black and Hispanic adults.
The VHA, “which provides health care services to 9 million veterans via VHA medical facilities (hereinafter referred to as facilities) across the country, is not immune to care access challenges,” the authors wrote. “The 2014 wait time scandal revealed excessive delays in care for veterans at some VHA facilities and highlighted the need for the VHA to improve timely access to care, especially for outpatient specialty care services. In response, the VHA adopted several policies aimed at improving care access, most significantly establishing the Veterans Choice Program (VCP) in 2014.”
With care paid for by the VHA, the VCP expanded opportunities for eligible veterans to receive care from community clinicians. “Since implementation of VCP, wait times have declined, and by 2017, the VHA generally had shorter wait times than those found in the private sector,” the study noted.
“Our own work examining wait times for five VHA outpatient specialty care services in 2015 and 2018 also reported declining wait times,” the authors added. “However, we additionally found wait time disparities: Black and Hispanic veterans had longer mean wait times for all five outpatient specialty care services studied. Other studies conducted both within and outside the VHA1 have noted similar care access disparities by race and ethnicity. However, these studies, like our own, do not capture the more recent operating environment, specifically the disruption in care access due to the COVID-19 pandemic and the implementation of the 2018 U.S. Department of Veterans Affairs (VA) Maintaining Internal Systems and Strengthening Integrated Outside Networks Act (MISSION), which further expanded veterans’ options to use community care.”
They pointed out that, while several studies have examined how COVID-19 altered healthcare patterns and utilization among VA-enrolled veterans, none appeared to have quantified the timeliness of care during COVID-19 or how the pandemic influenced care access disparities.
“In this cross-sectional study, wait-time disparities for outpatient cardiology and orthopedic services increased for Black and Hispanic veterans from the pre-COVID-19 to COVID-19 periods compared with white veterans,” the researchers concluded. “Specific facilities were identified where wait time disparities were higher, signaling potential opportunities for further investigation and intervention.”
- Gurewich D, Beilstein-Wedel E, Shwartz M, Davila H, Rosen AK. Disparities in Wait Times for Care Among US Veterans by Race and Ethnicity. JAMA Netw Open. 2023;6(1):e2252061. doi:10.1001/jamanetworkopen.2022.52061
