Rural Facilities Played a Disproportionate Role in Older Veteran Care
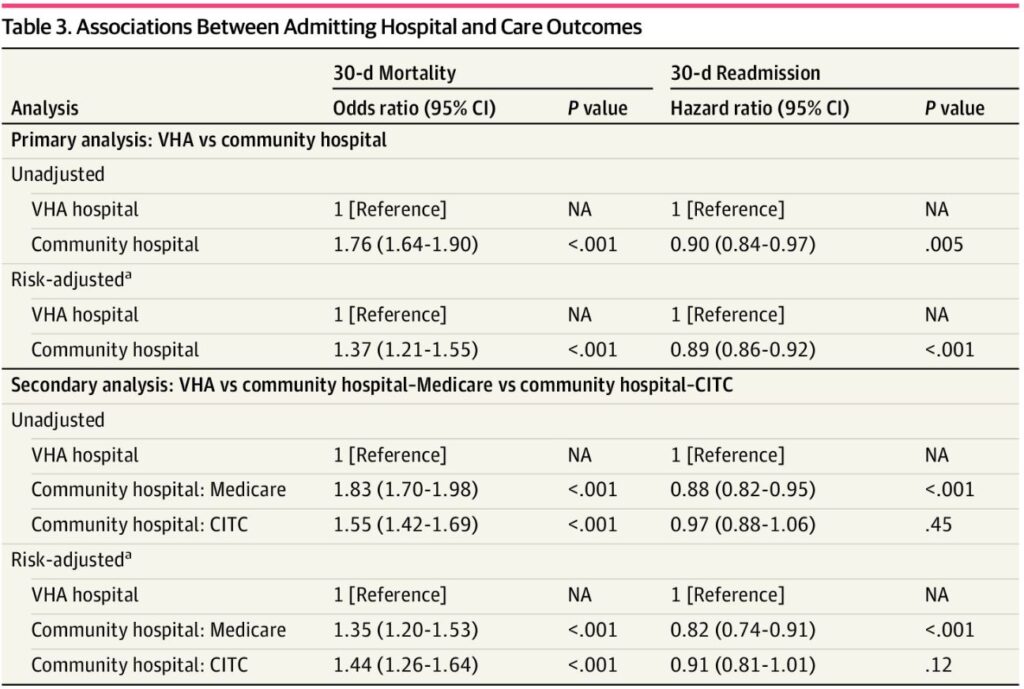
Click to Enlarge: Abbreviations: CITC, Care in the Community; NA, not applicable; VHA, Veterans Health Administration.
a) Adjusted for patient characteristics (ie, demographic characteristics, comorbidity, area-level social vulnerability, mechanical ventilation on admission, transfer in, rural residence, distance to nearest VHA and community hospital) using inverse probability of treatment weighting. Source: JAMA Network Open
IOWA CITY, IA – Veterans 65 and older with COVID-19 had lower survival rates when cared for in community hospitals than in VHA facilities. Contributing to the higher mortality rates, according to a recent study, is that so many older, rural veterans were treated by necessity in nearby hospitals.
“Compared with VHA hospitals, community hospitals played a disproportionate role in care for rural veterans with COVID-19, probably because of poor geographic access to VHA hospitals among rural veterans,” according to a recent study in JAMA Network Open.1
In fact, research led by the Iowa City VA Health Care System found that nearly half the community hospitals, 46.1%, caring for VHA enrollees with COVID-19 were in rural areas, and 24.7% were Critical Access Hospitals, a designation granted to small, rural hospitals to maintain their financial viability and preserve access to care in rural communities.
The study included 64,856 VHA enrollees aged 65 years or older and also enrolled in Medicare.
“The findings of this study suggest that it is important for the VHA to understand sources of COVID-19 mortality differences between VHA and community hospitals to plan care for VHA enrollees during future COVID-19 surges and the next pandemic,” the authors wrote.
They pointed out that, even though VHA enrollees received care for COVID-19 in both VHA and community hospitals, no much is known about the frequency or outcomes of care for veterans with COVID-19 in VHA vs. community hospitals.
In response, the study team sought to compare outcomes among veterans admitted for COVID-19 in VHA vs. community hospitals, using VHA and Medicare data from March 1, 2020, to Dec. 31, 2021. The focus was on hospitalizations for COVID-19 in 121 VHA and 4369 community hospitals in the United States.
Defined as the main outcomes of the retrospective cohort study were 30-day mortality and 30-day readmission.
The veterans’ mean [SD] age was 77.6, and 98.0% were men who were hospitalized for COVID-19. Most, 73.7%,) were admitted to community hospitals. Specifically:
- 56.1% were admitted to community hospitals via Medicare,
- 17.7% were admitted to community hospitals reimbursed via VHA’s Care in the Community program, and
- 26.3% were admitted to VHA hospitals.
Higher Mortality Rates
“Admission to community hospitals was associated with higher unadjusted and risk-adjusted 30-day mortality compared with admission to VHA hospitals (crude mortality, 12 951 of 47 821 [27.1%] vs, 3021 of 17 035 [17.7%]; P < .001; risk-adjusted odds ratio, 1.37 [95% CI, 1.21-1.55]; P < .001),” the researchers determined. “Readmission within 30 days was less common after admission to community compared with VHA hospitals (4898 of 38 576 [12.7%] vs 2006 of 14 357 [14.0%]; risk-adjusted hazard ratio, 0.89 [95% CI, 0.86-0.92]; P < .001).”
Background information in the articles noted that more than 90% of VHA enrollees aged 65 years or older are also enrolled in Medicare, and that the VHA has recently expanded efforts to pay community heathcare systems to provide services for VHA enrollees through the Care in the Community (CITC) program
“Available evidence indicates that veterans experience similar outcomes in VHA and community health care settings, although a recent study found better outcomes in VHA health care settings,” the authors advised.
They also noted the large surges in demand for acute hospital care created by the COVID-19 pandemic. The VHA’s 123 acute care hospitals in the United States have the capability of providing inpatient care for patients with severe COVID-19, but many VHA enrollees don’t have good geographic access to those hospitals. “More than one-third (41%) of VHA enrollees aged 65 years or older—a group at risk for severe COVID-19—live more than a 60-minute drive to the nearest acute care VHA hospital (M.E.O., unpublished data, January 3, 2023),” the authors explained. “In contrast, nearly all VHA enrollees aged 65 years or older (98%) live within a 60-minute drive to 1 of the approximately 4,400 community hospitals with acute care units in the U.S.”
The authors suggested that poor geographic access to VHA hospitals “means that community hospitals have likely played a large role in caring for acutely ill veterans with severe COVID-19…”
One result, according to the study, was that veterans experienced substantially higher risk-adjusted mortality in community hospitals than in VHA hospitals, although readmission was more common after VHA hospitalization.
“Our findings must be considered in the context of prior studies comparing the quality and outcomes of health care in VHA and non-VHA settings,” the authors pointed out. “Studies of care processes have generally found that the quality of VHA care compares favorably with non-VHA care, but studies of care outcomes have been mixed. Most prior studies compared outcomes for veterans receiving care in VHA facilities with outcomes for nonveterans receiving care in non-VHA facilities; these studies may have been biased if VHA enrollees tended to have worse health than the general population, as has been previously reported.”
Possible explanations for the finding of higher COVID-19 mortality in community hospitals compared with VHA hospitals included that the quality of care differed in VHA and community hospital settings,” the authors posited. “Since the beginning of the COVID-19 pandemic, the VHA health care system has worked to rapidly implement advances in care according to the latest treatment guidelines, including use of antiviral medications, corticosteroids, and other anti-inflammatory medications for people with severe COVID-19,” they wrote.
The somewhat higher readmission rates after admission to VHA hospitals compared with community hospitals might have another explanation. “This difference was not sensitive to adjustment for patient characteristics, suggesting that higher readmission rates after admission to VHA hospitals may reflect a feature of the VHA care system and not case mix,” the study stated. “Other studies have reported higher readmission rates in VHA hospitals compared with community hospital. Higher readmission rates may partly result from VHA programs to track veterans and manage care transitions after hospital discharge.”
The researchers called, however, for future studies to assess whether higher readmission rates in VHA hospitals suggest an undesired outcome or a necessary aspect of efforts to improve access to primary care during care transitions.
“Rural hospitals are financially stressed and closing at high rates,” the authors pointed out. “It is important for the VHA to understand the role of rural community hospitals in acute care for rural VHA enrollees — both during surges in demand for care during pandemics and overall — so that the VHA can support and collaborate with these hospitals to maintain access to care for rural veterans.”
- Ohl ME, Richardson Miell K, Beck BF, et al. Mortality Among US Veterans Admitted to Community vs Veterans Health Administration Hospitals for COVID-19. JAMA Netw Open. 2023;6(5):e2315902. doi:10.1001/jamanetworkopen.2023.15902
