New Study Provides Objective Measure of Condition Affecting Veterans
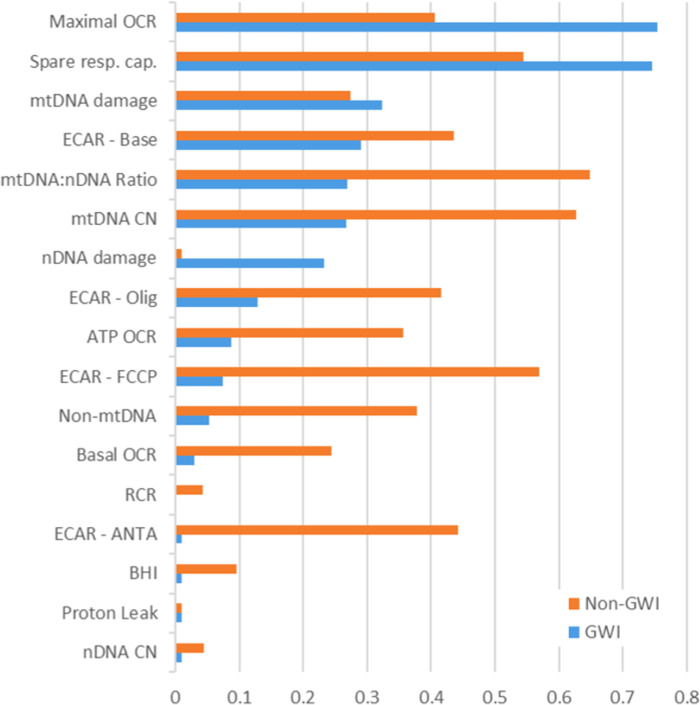
Click to Enlarge: Intraclass correlation coefficients by GWI status.
For graphing purposes, ICC estimates below zero were set to 0.01 Source: PLOS One
DURHAM, NC — The ability of white blood cells to make energy is significantly reduced in Gulf War Illness (GWI), which affects approximately 250,000 U.S. veterans, according to a new study finding a measurable biochemical difference in veterans who have the disease.
“Historically, GWI has been diagnosed based on a veteran’s self-reported symptoms, such as exercise-induced fatigue, indigestion, dizziness, insomnia, or memory problems. There’s been no objective biochemical or molecular measurements doctors could use to diagnose it,” explained study leader Joel Meyer, PhD, professor of environmental genomics at Duke’s Nicholas School of the Environment.
While measurements accessible in blood samples aren’t sufficient to serve as a stand-alone diagnostic test, those could be used to assess whether a prescribed treatment is working, Meyer said.
“Knowing this is an energetic deficiency can help us zero in on more effective ways to relieve the symptoms,” he added. “Blood tests, repeated over the course of the treatment, would show if a veteran’s white blood cells are responding to a treatment and producing more energy.”
The study, published in the open-access journal PLOS ONE, involved Duke, the VA’s War-Related Illness and Injury Study Center and the New Jersey Medical School at Rutgers.1
Researchers noted that GWI is a major health problem, but its etiology remained unclear. “We hypothesized that mitochondrial dysfunction is an important contributor to GWI, based on the similarity of some GWI symptoms to those occurring in some mitochondrial diseases; the plausibility that certain pollutants to which GW veterans were exposed affect mitochondria; mitochondrial effects observed in studies in laboratory models of GWI; and previous evidence of mitochondrial outcomes in studies in GW veterans,” they wrote.
The study team added that generating energy via oxidative phosphorylation is a primary role of mitochondria, but direct assessment of mitochondrial respiration, reflecting oxidative phosphorylation, had not been carried out in veterans with GWI.
In the case-control observational study, the researchers tested multiple measures of mitochondrial function and integrity in a cohort of 114 GW veterans, 80 with and 34 without GWI as assessed by the Kansas definition. For example, in circulating white blood cells, they analyzed multiple measures of mitochondrial respiration and extracellular acidification, which is a proxy for non-aerobic energy generation; mitochondrial DNA (mtDNA) copy number; mtDNA damage; and nuclear DNA damage.
Detailed Survey Data
Detailed survey data was collected on demographics; deployment; self-reported exposure to pesticides, pyridostigmine bromide and chemical and biological warfare agents; and current biometrics, health and activity levels. “We observed a 9% increase in mtDNA content in blood in veterans with GWI, but did not detect differences in DNA damage, the authors reported. “Basal and ATP-linked oxygen consumption were respectively 42% and 47% higher in veterans without GWI, after adjustment for mtDNA amount. We did not find evidence for a compensatory increase in anaerobic energy generation: extracellular acidification was also lower in GWI (12% lower at baseline).
With a subset of 27 and 26 veterans returning for second and third visits, respectively, allowed the study team to measure stability of mitochondrial parameters over time. While mtDNA CN, mtDNA damage, ATP-linked OCR, and spare respiratory capacity were moderately replicable over time, with intraclass correlation coefficients of 0.43, 0.44, 0.50, and 0.57, respectively, the researchers pointed out that other measures showed higher visit-to-visit variability. In fact, they noted that many measurements showed lower replicability over time among veterans with GWI compared to veterans without GWI.
“Finally, we found a strong association between recalled exposure to pesticides, pyridostigmine bromide, and chemical and biological warfare agents and GWI (p < 0.01, p < 0.01, and p < 0.0001, respectively),” according to the study. “Our results demonstrate decreased mitochondrial respiratory function as well as decreased glycolytic activity, both of which are consistent with decreased energy availability, in peripheral blood mononuclear cells in veterans with GWI.”
To determine if environmental factors might play a role, the researchers focused on the veterans’ surveys of self-reported symptoms and their written recollections of their deployments.
“We found veterans who recalled being exposed to pesticides and pyridostigmine bromide, a drug used during the Gulf War as a pretreatment to protect troops from the harmful effects of nerve agents, were more likely to get GWI after deployment,” Meyer said. “An interesting question is how these effects have persisted so long after the exposures.”
- Meyer JN, Pan WK, Ryde IT, Alexander T, Klein-Adams JC, Ndirangu DS, Falvo MJ. Bioenergetic function is decreased in peripheral blood mononuclear cells of veterans with Gulf War Illness. PLoS One. 2023 Nov 1;18(11):e0287412. doi: 10.1371/journal.pone.0287412. PMID: 37910447; PMCID: PMC10619881.
