COVID-19 Pandemic Significantly Worsened the Situation
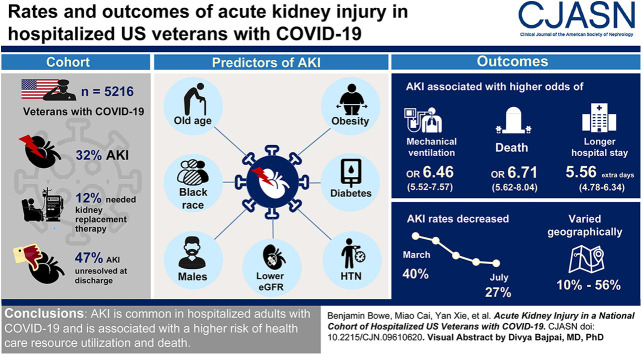
Click To Enlarge: Trajectories of serum creatinine among a cohort of US veterans hospitalized with coronavirus disease 2019 who were discharged alive. (A) Fourteen and (B) 30 days. Baseline serum creatinine is included at time −1. Trajectories are colored by AKI status and severity. In those who received KRT, the serum creatinine trajectory was censored at the time of KRT. Bands represent the 95% confidence intervals.
DETROIT — More than a quarter of patients with acute kidney injury died within a year of hospitalization at the VHA, according to a 10-year study that ended in late 2017.
AKI, an abrupt decline in kidney function, is a frequent complication in hospitalized patients, and an analysis recently published in the Clinical Journal of the American Society of Nephrology revealed that the healthcare system serving veterans had a high mortality rate from the condition.1
The study team led by Ryann Sohaney, DO, of the Henry Ford Health System in Detroit and the University of Michigan in Ann Arbor, calculated recent short- and long-term mortality trends in hospitalized patients with AKI, analyzing data from the VHA on all patients hospitalized from Oct. 1, 2008, to Sept. 31, 2017.
With 1.7 million patients and 2.7 million hospitalizations across the study period, researchers determined that 6% of AKI patients died in-hospital, and 28% died within a year. For inpatients without AKI, in-hospital and one-year mortality was 0.8% and 14%, respectively, according to the report.
While the VA has made significant efforts to turn those numbers around, the COVID-19 pandemic has only increased cases and erased a lot of progress in the ensuing years, according to other research.
“Our study indicates that AKI-associated mortality remains high, as greater than 1 in 4 patients died within 1 year. There has been no significant progress toward improving in-hospital or long-term AKI survivorship,” Sohaney said.
An earlier version of the study published as a research letter last August by the National Kidney Foundation pointed out that diagnostic coding of AKI substantially increased at the VHA, with the authors noting, “Because payment for services is unaffected by diagnostic coding within the VHA, these findings likely represent improved AKI recognition. Further studies are needed to examine whether this has resulted in clinical outcome improvements among patients with AKI. Although AKI by diagnosis code increased across all KDIGO AKI stages, the relative increase in coding was greatest for stages 1 and 2. This is important because even mild AKI associates with adverse outcomes such as incident CKD.”
It added that the Kidney Disease Improving Global Outcomes AKI guideline recommends evaluating patients three months after diagnosis to assess for resolution or new onset or progression of CKD. “However, in this VHA cohort, only half the AKI episodes defined by [serum creatinine} had an accompanying diagnosis code, with <75% coding even for severe (stage 3) AKI. Improved awareness of AKI is a critical first step in ensuring appropriate follow-up.”
The authors added, “Another key finding of this study is the stable temporal incidence of AKI-D. This contrasts with a previous study reporting an increase in AKI-D of ∼10% per year in 2000-2009.”
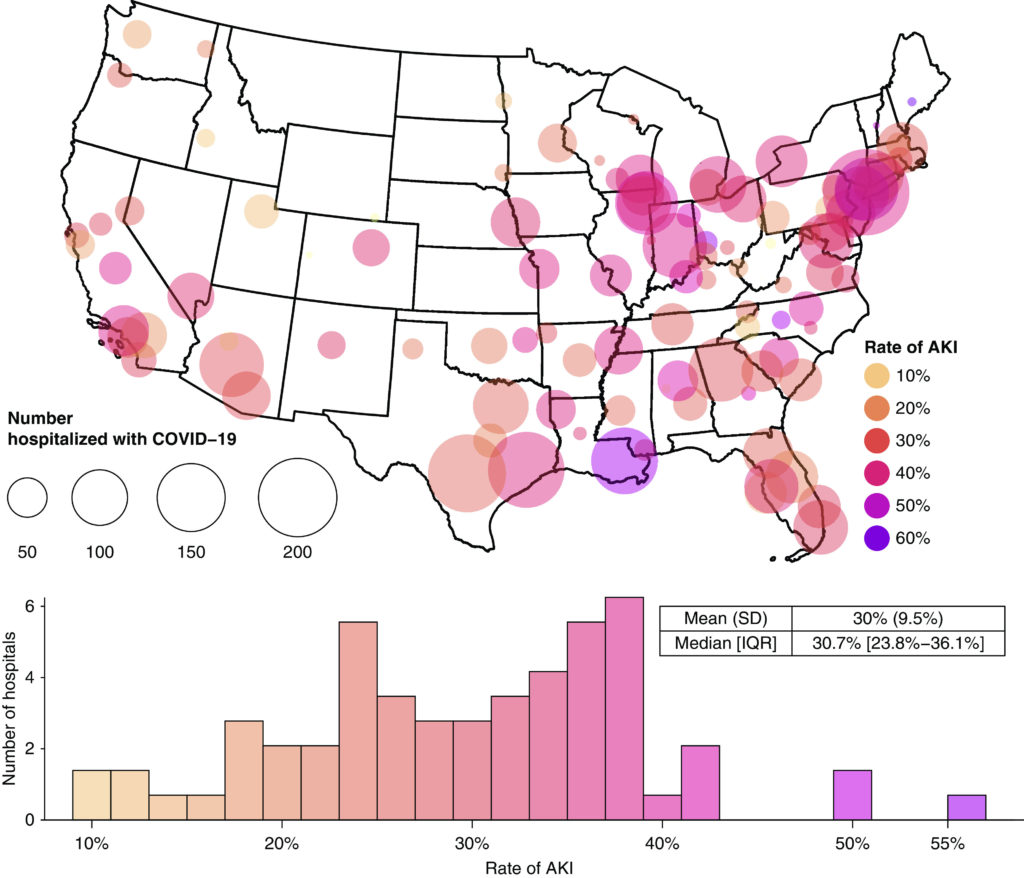
Click To Enlarge: Map of the geographic distribution of participants hospitalized with coronavirus disease 2019 (COVID-19) in Veterans Affairs (VA) facilities. The size of the circle represents the absolute number of participants hospitalized with COVID-19 in a VA hospital system. The color gradient represents the rates of AKI among those hospitalized for COVID-19, expressed as a percentage. The histogram shows the distribution of rates across hospital systems, and descriptive statistics for this distribution are presented. Hospital systems with <20 participants with COVID-19 are excluded from the histogram. IQR, interquartile range.
“The rapid increase in diagnostic coding suggests improving clinician recognition of AKI, an essential component for targeting patients for outpatient follow-up and may have implications for improving long-term AKI outcomes. At the same time, it is disappointing that, even after adjusting for comorbid conditions, there have been only modest changes in AKI incidence during the past decade, suggesting much room for improvement,” the authors concluded.
In the more recently published studies, they asserted, “Over the past decade, there seems to have been no significant progress toward improving in-hospital or long-term AKI survivorship.”
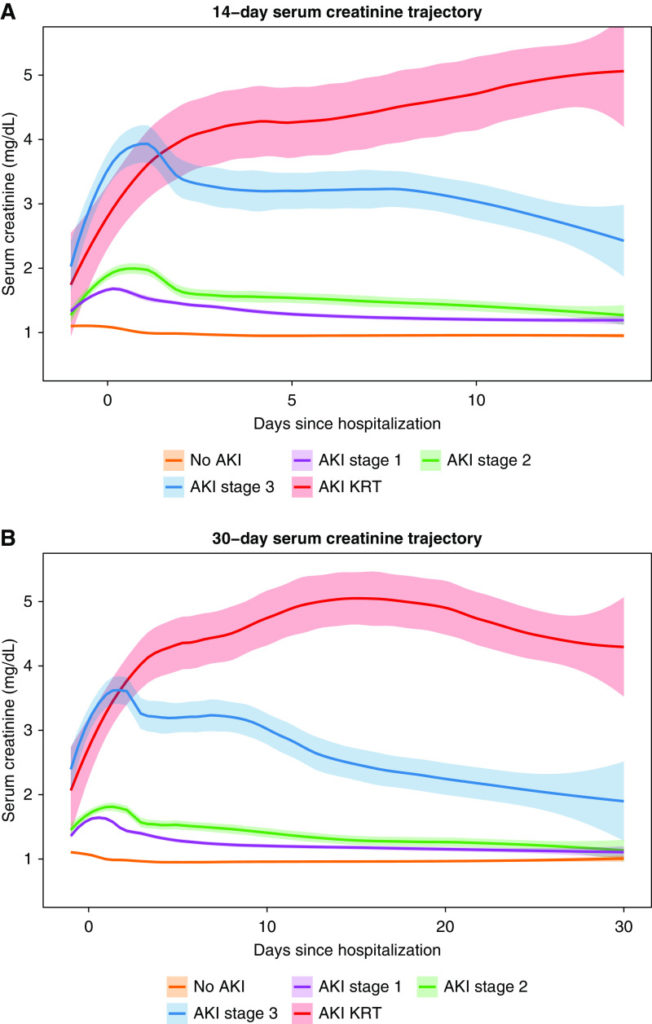
A journal article published at the end of last year by researchers from the St. Louis VA Healthcare System noted that the COVID-19 pandemic has only exacerbated problems with AKI. In a study also published in CJASN, the study team focused on a cohort of 5,216 veterans hospitalized with COVID-19 identified through July 23, 2020. 2
Of those, 32% had AKI. Furthermore, according to the authors, 58%), 13% and 16% met Kidney Disease Improving Global Outcomes definitions of stage 1, 2, and 3 AKI, respectively, and 12% received kidney replacement therapy.
In fact, the study pointed out that 8% of participants had AKI within one day of hospitalization, and 47% did not recover to baseline serum creatinine by discharge. Significant predictors of AKI during hospitalization with COVID-19 were older age, Black race, male gender, obesity, diabetes, hypertension and lower eGFR.
In that study, AKI was also associated with a higher risk of death (odds ratio, 6.71; 95% confidence interval, 5.62 to 8.04). The researchers noted that the association with mortality was stronger in Blacks (P value of interaction <0.001).
“Hospital-level rates of AKI exhibited substantial geographic variability, ranging from 10% to 56%,” the authors explained. “Between March and July 2020, AKI rates declined from 40% to 27%; proportions of AKI stage 3 and AKI requiring KRT decreased from 44% to 17%. Both geographic and temporal variabilities were predominately explained by percentages of Blacks (31% and 49%, respectively).”
AKI also was found to be associated with higher mechanical ventilation use (odds ratio, 6.46; 95% confidence interval, 5.52 to 7.57) and longer hospital stay (5.56 additional days; 95% confidence interval, 4.78 to 6.34).
The study concluded, “AKI is common during hospitalization with COVID-19 and associated with higher risk of health care resource utilization and death. Nearly half of patients with AKI did not recover to baseline by discharge. Substantial geographic variation and temporal decline in rates and severity of AKI were observed.”
The VHA has a National Kidney Program to improve quality of healthcare services delivered to veterans with kidney disease. The program supplies kidney-related services to VA dialysis centers and provides health care providers with education, research and informatics resources.
- Sohaney R, Yin H, Shahinian V, Saran R, Burrows NR, Pavkov ME, Banerjee T, Hsu CY, Powe N, Steffick D, Zivin K, Heung M; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team. In-Hospital and 1-Year Mortality Trends in a National Cohort of US Veterans with Acute Kidney Injury. Clin J Am Soc Nephrol. 2022 Feb;17(2):184-193. doi: 10.2215/CJN.01730221. PMID: 35131927.
- Bowe B, Cai M, Xie Y, Gibson AK, Maddukuri G, Al-Aly Z. Acute Kidney Injury in a National Cohort of Hospitalized US Veterans with COVID-19. Clin J Am Soc Nephrol. 2020 Dec 31;16(1):14-25. doi: 10.2215/CJN.09610620. Epub 2020 Nov 16. PMID: 33199414; PMCID: PMC7792643.
- Sohaney R, Yin H, Shahinian V, Steffick, et. al. Trends in the Incidence of Acute Kidney Injury in a National Cohort of US Veterans. AJKD. Published August 05, 2020. https://doi.org/10.1053/j.ajkd.2020.05.027