GRONINGEN, THE NETHERLANDS — Could high levels of the chemokine TARC produced in tumor cells in classic Hodgkin lymphoma help predict the malignancy?
A new article in the journal Blood suggested that could be possible, noting TARC levels measured in prediagnostic serum samples found notably increased values in most patients more than six years before diagnosis.1
The Walter Reed Army Institute of Research in Silver Spring, MD, participated in the research, which was led by University Medical Center in Groningen, the Netherlands.
Background information in the study pointed out that classic Hodgkin lymphoma (HL) is a common cancer in young adults, especially in Western industrialized countries. Its tumor cells, which derive from germinal center B cells, are called Hodgkin and Reed-Sternberg (HRS) cells. In nearly all patients, more than 90%, the HRS cells express thymus and activation-related chemokine (TARC), also known as CC chemokine ligand 17 (CCL17). , The chemokine attracts CC chemokine receptor type 4 (CCR4) positive CD4 T cells which may form characteristic T cell rosettes surrounding individual HRS cells and .2 provide essential stimulation to antigen presenting B cells.
“Immunohistochemistry shows that TARC is exclusively expressed by HRS cells, while it is not detectable in the abundant and heterogeneous HL tumor microenvironment, nor in the vast majority of other lymphomas,” the authors explained. “The prolific production of TARC by HRS cells is reflected by increased serum levels at the time of diagnosis. These levels are often more than 100 times higher than in healthy controls and are strongly associated with tumor volume, disease stage, and response to therapy. Hence, serum TARC (sTARC) levels largely reflect presence and abundance of HRS cells.”
For the current study, the researchers hypothesized that sTARC levels are elevated in samples collected prior to diagnosis. To determine whether that was the case, they selected samples from the DoD’s Serum Repository, which harbors a prospective collection of millions of specimens from U.S. active-duty military personnel.
Included were all servicemembers with an initial diagnosis of HL identified between 1990 and 2000 and with at least one pre-diagnostic serum sample in the 10 years before diagnosis were included. Pathology review confirmed 103 HL cases, of which 23 were positive for tumor cell Epstein Barr virus (EBV) based on in situ hybridization for EBV encoded RNAs and/or immunohistochemistry for latent membrane protein-1.
Histology subtypes were nodular sclerosis, mixed cellularity, and classic not otherwise specified.
For each case, two precisely matched controls were selected from the DoD Serum Repository based on age, sex, race and ethnicity, number of serum samples, and sample draw date (+/- 30 days for each sample). The median age was 26 years (range 18–51 years) and 10% of patients were female.
The research team measured TARC levels with a Luminex assay.
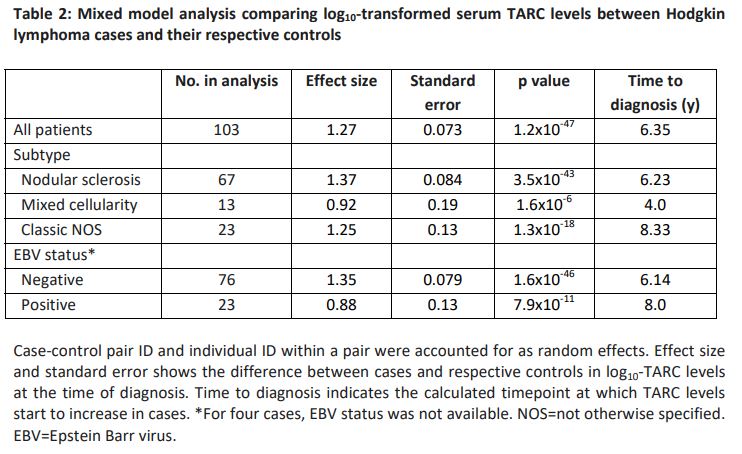
“The temporal distribution of sTARC values showed clear differences between cases and controls both for histology subtypes and for subgroups defined by tumor cell EBV status,” the study noted. “Over the entire time span of 10 years prior to diagnosis, the collective sTARC levels in cases (median 1305 pg/ml, max. 1.5×105) were higher than those in controls (median 407 pg/ml, max. 2.1×103 ; p=2.1×10-25). The mixed model analysis on cases and their respective two matched controls was even more significant. The corresponding log10 effect size of 1.27 indicates an estimated 18.6-fold higher sTARC level in cases compared to respective controls at the time of diagnosis (95% CI 13.4-25.9).”
The researchers advised that the largest effect sizes were observed for nodular sclerosis and EBV negative HL cases (23.3 and 22.5-fold increase, respectively). They also found that sTARC levels in the smaller mixed cellularity and EBV positive subgroups were notably increased at diagnosis (estimated 8.2 and 7.6-fold increase, respectively) with no confounding effects of age and sex.
In fact, the study found that the mixed-model analysis per time interval before diagnosis was significant until five years before diagnosis.
“Log10-transformed sTARC levels increased by 0.20 per year in cases compared to controls, indicating a 1.6-fold rise in sTARC levels every year,” the authors explained. “This means that sTARC levels start to increase 6.35 years before diagnosis, with some variability in specific HL subsets. The young adult age incidence peak is characteristic of HL, but for many of the cases in our study, sTARC levels were already rising between the ages of 15 to 20 years. TARC is not secreted by normal B cells, leading us to speculate that the events initiating the development of HRS cells occur even earlier, likely during childhood.”
The study team posited that initiating events might have involved delayed common respiratory infections in childhood, which is strongly associated with the young adult HL incidence peak in Western industrialized countries, especially if the respiratory infections induce activation of regional lymph nodes in the head and neck region or the mediastinum, typical locations of HL manifestation.
- Diepstra A, Nolte IM, van den Berg A, Magpantay LI, Martinez-Maza O, Levin LI. Elevated serum TARC levels precede classic Hodgkin lymphoma diagnosis by several years. Blood. 2023 Sep 25:blood.2023020959. doi: 10.1182/blood.2023020959. Epub ahead of print. PMID: 37748137.