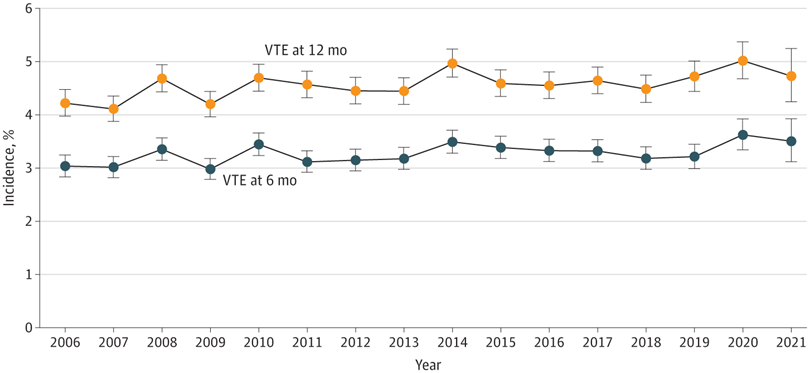
Click to Enlarge: VTE events were captured using a rigorously validated algorithm and based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes, anticoagulant medications, and natural language processing radiology reports in inpatient and outpatient encounters. Dots denote means and error bars denote 95% CIs. Source: JAMA Network Open
PORTLAND, OR — Has cancer-directed therapy changed patterns of the incidence and risk of cancer-associated thrombosis (CAT) at the VA?
That was the question raised in a cohort study of 434,203 veterans with solid tumors and hematologic neoplasms within the VHA.
Oregon Health & Science University Researchers and colleagues found a high incidence of CAT, with yearly trends ranging stably from 4.2% to 4.7% over the 16-year study period. They also determined that cancer type and stage and systemic treatment were significantly associated with CAT and that risk varied among patients of different races and ethnicities.
“These findings suggest that patient-specific and treatment-specific factors, accounting for changes in the treatment landscape over time, warrant consideration in future venous thromboembolism risk stratification models,” the authors wrote in JAMA Network Open.1
The study team pointed out the importance of identifying changes in epidemiologic patterns of the incidence and risk of cancer-associated thrombosis (CAT), particularly with evolving cancer-directed therapy.
The longitudinal, retrospective cohort study was conducted from 2006 to 2021, and the duration of follow-up was from the date of diagnosis until the first venous thromboembolism (VTE) event, death, loss of follow-up (defined as a 90-day gap without clinical encounters) or administrative censoring on April 1, 2022. Included in the study were patients with newly diagnosed invasive solid tumors and hematologic neoplasms, with data analyzed from December 2022 to February 2023.
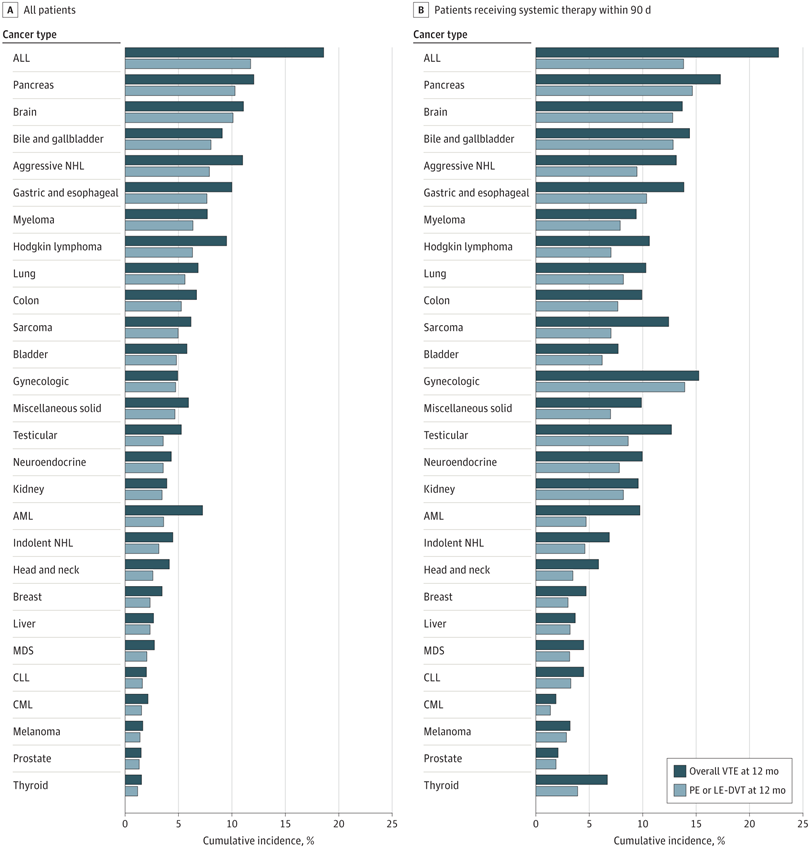
Click to Enlarge: Panel A shows cumulative incidence of VTE at 12 months among all patients in the cohort stratified by cancer type, and panel B shows cumulative incidence of VTE at 12 months among patients who received systemic therapy within 3 months of diagnosis stratified by cancer type. ALL indicates acute lymphoblastic leukemia; AML, acute myeloid leukemia; CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; LE-DVT, lower extremity deep venous thrombosis; MDS, myelodysplastic syndrome; NHL, non-Hodgkin lymphoma; and PE, pulmonary embolism. Source: JAMA Network Open
The researchers assessed the incidence of VTE using a combination of the International Classification of Diseases, Ninth Revision, Clinical Modification and International Statistical Classification of Diseases, Tenth Revision, Clinical Modification and natural language processing confirmed outcomes. Taken into consideration were patient variables, including demographics, region, rurality, area deprivation index, National Cancer Institute comorbidity index, cancer type, staging, first-line systemic treatment within 3 months (time-varying covariate) and other factors that could be associated with the risk of VTE.
Participants had a median age of 67 and were 72.1% white, 20.6% Black, 4.7% Hispanic and 1.7% Asian or Pacific Islanders.
Results indicated that the overall incidence of CAT at 12 months was 4.5%, with yearly trends ranging from 4.2% to 4.7%.
“The risk of VTE was associated with cancer type and stage. In addition to confirming well-known risk distribution among patients with solid tumors, a higher risk of VTE was observed among patients with aggressive lymphoid neoplasms compared with patients with indolent lymphoid or myeloid hematologic neoplasms,” the study authors pointed out.
Compared with no treatment, patients receiving first-line chemotherapy (hazard ratio [HR], 1.44; 95% CI, 1.40-1.49) and immune checkpoint inhibitors (HR, 1.49; 95% CI, 1.22-1.82) had a higher adjusted relative risk than patients receiving targeted therapy (HR, 1.21; 95% CI, 1.13-1.30) or endocrine therapy (HR, 1.20; 95% CI, 1.12-1.28), according to the report, which also noted that adjusted VTE risk was significantly higher among non-Hispanic Black patients (HR, 1.23; 95% CI, 1.19-1.27) and significantly lower in Asian or Pacific Islander patients (HR, 0.84; 95% CI, 0.76-0.93) compared with Non-Hispanic white patients.
“In this cohort study of patients with cancer, a high incidence of VTE was observed, with yearly trends that remained stable over the 16-year study period,” the researchers concluded. “Both novel and known factors associated with the risk of CAT were identified, providing valuable and applicable insights in this current treatment landscape.”
Background information in the study advised that VTE is one of the leading causes of noncancer-related mortality in patients with active cancer receiving systemic therapy.
“Patients with cancer are not only at increased risk of VTE compared with the general population, but also at higher risk of VTE recurrence despite receipt of anticoagulation therapy,” the article states. “Our understanding of the pathophysiology of cancer-associated thrombosis (CAT) has evolved over the past few decades, as have validated tools to identify those at high risk.8 Despite these advances, there remains a critical need to identify the associations of race and ethnicity, cancer subtype, and systemic therapy regimens with CAT, particularly over time as the landscape of antineoplastic therapies has evolved.”
- Martens KL, Li A, La J, et al. Epidemiology of Cancer-Associated Venous Thromboembolism in Patients With Solid and Hematologic Neoplasms in the Veterans Affairs Health Care System. JAMA Netw Open. 2023;6(6):e2317945. doi:10.1001/jamanetworkopen.2023.17945

