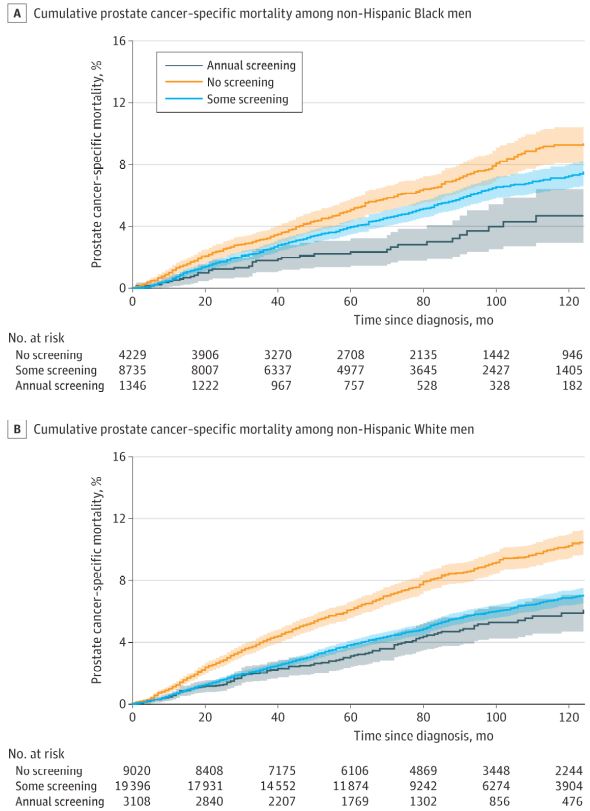
Click to Enlarge: Prostate Cancer–Specific Mortality Among Non-Hispanic Black Men and Non-Hispanic White Men. Shaded areas indicate 95% CIs. Source: JAMA Oncology
LA JOLLA, CA — The benefits of annual prostate-specific antigen screening (PSA) appear to vary by race, decreasing the risk of prostate cancer-specific mortality among non-Hispanic Black men but not non-Hispanic white men, according to a new veteran study.
The study of 45,800 U.S. veterans indicated that PSA screening generally was associated with reduced risk of prostate cancer-specific mortality (PCSM) among both groups. The report in JAMA Oncology noted, however, that, compared with less-frequent screening, annual screening was associated with decreased risk of PCSM among Black men but not among white men.1
The researchers from the University of California, San Diego in La Jolla, and the VA San Diego Healthcare System advised that annual screening may be particularly important for Black men, adding that more-intensive screening protocols may benefit Black patients, but more research is necessary “to identify appropriate protocols to maximize the benefits of PSA screening.”
Background information in the article pointed out that Black men have higher prostate cancer incidence and mortality than non-Hispanic white men. Yet, the authors added, “Black men have been underrepresented in clinical trials of prostate-specific antigen (PSA) screening; thus, there is a lack of data to guide screening recommendations for this population.”
The authors suggested, “Black men have higher prostate cancer-specific mortality (PCSM) compared with non-Hispanic White men, likely reflecting systemic inequities in health care access and delivery, social determinants of health, and possible differences in tumor biology. Prostate-specific antigen screening among Black men may be associated with reductions in these disparities in mortality. However, more data on screening are needed to develop appropriate, personalized recommendations for Black men.”
They defined the study objective as investigating whether previous PSA screening was associated with decreased PCSM risk among non-Hispanic Black men and non-Hispanic white men with prostate cancer in a racially diverse cohort of U.S. veterans The retrospective cohort study used data from the VHA’s Informatics and Computing Infrastructure for more than 45,000 men aged 55 to 69 years who were diagnosed with intermediate-, high- or very high-risk prostate cancer from Jan. 1, 2004, to Dec.31, 2017. Participants all self-identified as non-Hispanic Black or non-Hispanic white. Data were analyzed from August 2021 to March 2022.
The focus was on the patients’ prostate-specific antigen screening rates, defined as the percentage of years in which PSA screening was conducted during the five years before diagnosis of prostate cancer.
Researchers assessed the risk of PCSM, classifying patients as having no prior PSA screening, some screening (less than annual) or annual screening in the five years before diagnosis.
Participants were 45,834 veterans with a mean age of 62.7. About 31% were non-Hispanic Black men, while the remaining 69% were non-Hispanic white men.
Results indicated that the PSA screening rate was associated with a lower risk of PCSM among Black men (subdistribution hazard ratio [sHR], 0.56; 95% CI, 0.41-0.76; P = 0.001) and white men (sHR, 0.58; 95% CI, 0.46-0.75; P = 0.001). Subset analysis revealed, however, that, annual screening (versus some screening) was associated with a significant reduction in risk of PCSM among Black men (sHR, 0.65; 95% CI, 0.46-0.92; P = 0.02) but not among white men (sHR, 0.91; 95% CI, 0.74-1.11; P = 0.35).
“In this cohort study, PSA screening was associated with reduced risk of PCSM among non-Hispanic Black men and non-Hispanic white men,” the authors pointed out. “Annual screening was associated with reduced risk of PCSM among Black men but not among white men, suggesting that annual screening may be particularly important for Black men.”
Younger at Diagnosis
The researchers pointed out that their results for white men are consistent with those of a pooled analysis of previous randomized clinical trials, noting, “However, those trials were conducted in predominantly white populations. Given that Black men are younger at diagnosis and have worse prostate cancer survival compared with white men, customized screening recommendations may be beneficial in this population.”
They cited recent research from some of the same authors indicating that screening was associated with reduced PCSM among younger Black veterans age 40-55 years, pointing out, “The present analysis suggests that these findings are also applicable to older Black men in a similar age range as those in the aforementioned screening trials.”
The researchers called their results “biologically plausible because a shorter screening interval may be valuable for detecting aggressive disease, which is more common in Black men.”
- Sherer MV, Qiao EM, Kotha NV, Qian AS, Rose BS. Association Between Prostate-Specific Antigen Screening and Prostate Cancer Mortality Among Non-Hispanic Black and Non-Hispanic White US Veterans. JAMA Oncol. Published online Aug. 04, 2022. doi:10.1001/jamaoncol.2022.29702.
- Qiao EM, Lynch JA, Lee KM, Kotha NV, Nalawade V, et. al. Evaluating Prostate-Specific Antigen Screening for Young African American Men With Cancer. J Natl Cancer Inst. 2022 Apr 11;114(4):592-599. doi: 10.1093/jnci/djab221. PMID: 34893859; PMCID: PMC9002290.

