Disparities Found in Usually Equal-Access Healthcare System
SAN DIEGO — The U.S. Military Health System is touted as an equal-access medical provider, and scores of studies have demonstrated that few racial inequities exist in the treatment it provides for many conditions.
In an exception to the usual, however, an analysis determined that white patients are much more likely to receive knee arthroplasty within three years of osteoarthritis when other treatments received—e.g. physical therapy or medications—are considered.
The study was conducted by researchers from the Naval Medical Center in San Diego, Brooke Army Medical Center at Fort Sam Houston, TX, and the Uniformed Services University for the Health Sciences and the Henry M. Jackson Foundation for the Advancement of Military Medicine Inc. both in Bethesda, MD. Results were published in the journal Arthritis Care and Research.1
The retrospective observational cohort study used medical record data of 29,374 patients who received a primary osteoarthritis diagnosis in the MHS between January 2016 and January 2020. Researchers analyzed data including receipt of physical therapy one-year prediagnosis and up to three years post-diagnosis, pre-diagnosis opioid and nonopioid prescription receipt, health-related factors associated with levels of racism and the primary outcome, knee arthroplasty receipt within three-years post-diagnosis.
“In a generalized additive model with time-varying covariates, Asian and Pacific Islander (Incidence Rate Ratio (IRR) 0.58; 95% CI 0.45, 0.74), Black (IRR 0.52; 95%CI 0.46, 0.59), and Latinx (IRR 0.66; 95%CI 0.52, 0.85) patients experienced racialized inequities in knee arthroplasty receipt, relative to white patients (all p < 0.001),” the study authors reported.
The researchers advised that, in their findings, Asian and Pacific Islander, Black and Latinx patients “were significantly less likely to receive a knee arthroplasty, relative to white patients. Taken together, system-level resources are needed to identify and address mechanisms underlying institutional inequities in knee arthroplasty receipt, such as factors related to systemic and structural, institutional, and personally-mediated racism.”
Volume Improves Outcomes
In an interesting twist, another recent study urged that more TKAs—as well as total hip arthroplasties (THAs)—be performed within the MHS instead of the increasing use of outside care. The study found that higher volumes are associated with better overall care.
The research, led by Baylor University in Waco, TX, and including participation from the Uniformed Services University of the Health Sciences, was published in Military Medicine.2
As with the VA, the DoD “is reforming the military health system where surgeries are increasingly referred from military treatment facilities (MTFs) with direct care to higher-volume civilian hospitals under purchased care,” the authors wrote. “This shift may have implications on the quality and cost of care for TRICARE beneficiaries.”
To find out, the researchers examined the impact of care source and surgical volume on perioperative outcomes and cost of and TKAs.
TRICARE claims were examined for patients who underwent THA or TKA between 2006 and 2019. The researchers evaluated the 30-day readmissions, complications and costs between direct and purchased care using the logistic regression model for surgical outcomes and generalized linear models for cost.
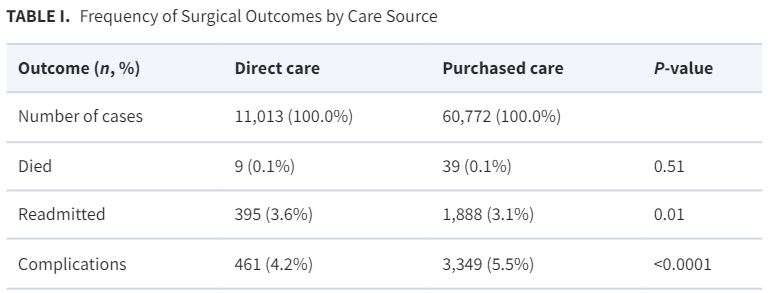
Included in the study were 71,785 TKA and THA procedures. The 11,013 (15.3%) that were performed in direct care had higher odds of readmissions (odds ratio, OR 1.29 [95% CI, 1.12-1.50]; P < 0.001) but fewer complications (OR 0.83 [95% CI, 0.75-0.93]; P = 0.002).
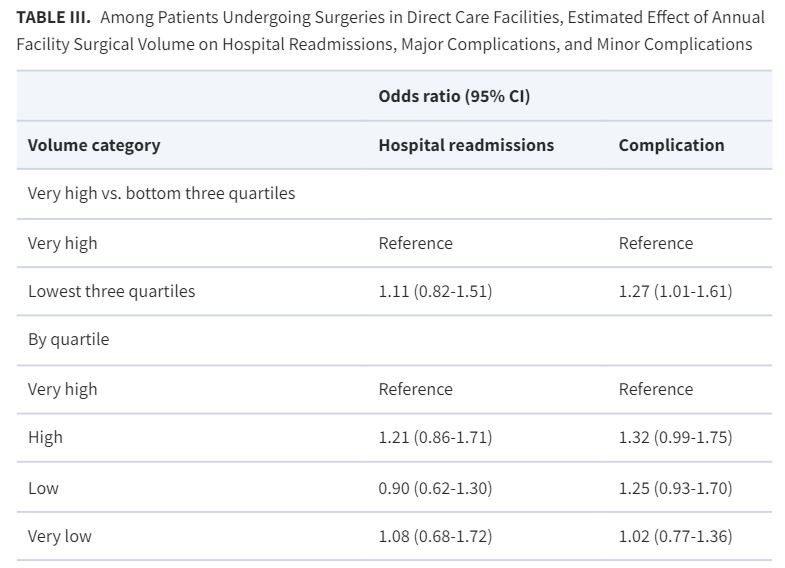
“Within direct care, lower-volume facilities had more complications (OR 1.27 [95% CI, 1.01-1.61]; P = 0.05),” the researchers explained. “Costs for index surgeries were significantly higher at MTFs $26,022 (95% CI, $23,393-$28,948) vs. $20,207 ($19,339-$21,113). Simulating transfer of care to very high-volume MTFs, estimated cost savings were $4,370/patient and $20,229,819 (95% CI, $17,406,971-$25,713,571) in total.”
The study concluded that MTFs are associated with lower odds of complications, higher odds of readmission and higher costs for THA and TKA compared to purchased care facilities. “These findings mean that care in the direct setting is adequate and consolidating care at higher-volume MTFs may reduce health care costs,” according to the researchers.
- Sowa H, Patzkowski J, Ismawan J, Velosky AG, Highland KB. Racialized Inequities in Knee Arthroplasty Receipt After Osteoarthritis Diagnosis in the US Military Health System. Arthritis Care Res (Hoboken). 2024 Jan 7. doi: 10.1002/acr.25290. Epub ahead of print. PMID: 38185854.
- Haag A, Hosein S, Lyon S, Labban M, Wun J, Herzog P, Cone EB, Schoenfeld AJ, Trinh QD. Outcomes for Arthroplasties in Military Health: A Retrospective Analysis of Direct Versus Purchased Care. Mil Med. 2023 Nov 8;188(Suppl 6):45-51. doi: 10.1093/milmed/usac441. PMID: 37948209.