Click To Enlarge: Source: Parikh TJ, Stryczek KC, Gillespie C, Sayre GG, Feemster L, Udris E, Majerczyk B, Rinne ST, Wiener RS, Au DH, Helfrich CD. Provider anticipation and experience of patient reaction when deprescribing guideline discordant inhaled corticosteroids. PLoS One. 2020 Sep 17;15(9):e0238511.
SAN FRANCISCO — Clinicians are often wary of suggesting that older patients discontinue some of their medications, believing they will get pushback.
A recent study involving the San Francisco VAMC suggested, however, that likely would not be the case. The report in the Journal of the American Geriatric Society found that older adults with probable or possible dementia are quite willing to cut back on medications if advised to do so.1
The authors reported that, in a survey they conducted, 87% of seniors with suspected cognitive issues said they would drop at least one medication “if their doctor said it was possible.” That increased to 92% among those who were taking six or more medications.
The findings confirmed that patients and their families tend not to be barriers to deprescribing.
While 58% of the 422 older adults had probable or possible dementia, most also had otherwise good to excellent health, according to the report. Still, more than half was being treated with polypharmacy—taking six or more regular medications.
Deprescribing could be especially important in the case of these patients, the San Francisco VAMC-led researchers pointed out, because some of the drugs might be exacerbating cognitive symptoms, causing poor outcomes and resulting in adverse drug reactions—in addition to the added costs.
The national sample represented 1.8 million Medicare beneficiaries and was recruited by the National Health and Aging Trends Study (NHATS). Most respondents, about three-quarters, were 75-plus. Overall, 44% had possible dementia, and 56% had probable dementia as determined by NHATS criteria, the researchers noted.
In addition to adverse interactions and outcomes, polypharmacy also “contributes to challenges with adherence, since more complicated medication regimens require more time and attention, and increase the potential for making mistakes and inadvertent misuse,” said first author Matthew Growdon, MD, an aging research fellow at the San Francisco VAMC and the University of California San Francisco’s Division of Geriatrics.
“Many drugs may be especially harmful to older adults with cognitive impairment, such as benzodiazepines, used to treat anxiety, and oxybutynin, used to treat urinary incontinence. These drugs have sedating effects that increase the risk of delirium and can worsen dementia,” Growdon pointed out.
Participants taking six or more pills also were more willing to drop one; 29% in this group agreed “that at least one medication was no longer necessary” compared with 13% in those taking less than six pills.
Growdon suggested the high rate of subscribing is linked to “a biomedical culture of prescribing,” as well as “deference on the part of patients and physicians to the prescribing physician.”
Co-author Michael Steinman, MD, also of the UCSF Division of Geriatrics and the San Francisco VAMC, added, “Additionally, treatment of cognitive impairment itself and its complications may lead to more medication use. This can include medications to help with memory and with mood and medications for symptoms that people with cognitive impairment can increasingly face, like urinary incontinence.”
Vitamin D and calcium and medications for high blood pressure, diabetes, constipation and arthritis were among other commonly prescribed or recommended drugs, the authors noted.
Furthering Goals
“Our aim as geriatricians is to prescribe medications to help older people achieve their health and function goals, especially those with dementia,” said co-senior author Kenneth Boockvar, MD, from the James J. Peters VAMC in Bronx, NY, the New Jewish Home and Icahn School of Medicine at Mount Sinai. “We need to avoid or stop taking medications that do not further those goals. That’s where deprescribing comes in.”
Deprescribing is about medical optimization, “rather than taking away medications,” said Growdon. “We should strive to ensure that the benefits outweigh risks and that we are prescribing in line with goals of care and taking into consideration factors in older adults, like frailty, multimorbidity, cognitive impairment and functional status. One thing this study can hopefully add is that patient/family resistance to deprescribing should not be seen as a barrier.”
A 2020 study led by researchers from the Seattle-Denver Center of Innovation for Veteran-Centered & Value-Driven Care at the VA Puget Sound Healthcare System in Seattle, WA, foreshadowed the recent findings. The VA Northeast Ohio Healthcare System in Cleveland and the Center for Healthcare Organization & Implementation Research at the Edith Nourse Rogers Memorial Veterans Hospital in Bedford, MA4, also participated in the research, as did researchers from the University of Washington in Seattle.2
The study team “sought to understand veteran and provider experience when de-implementing guideline-discordant use of inhaled corticosteroids (ICS) in those with mild-to-moderate chronic obstructive pulmonary disease (COPD).”
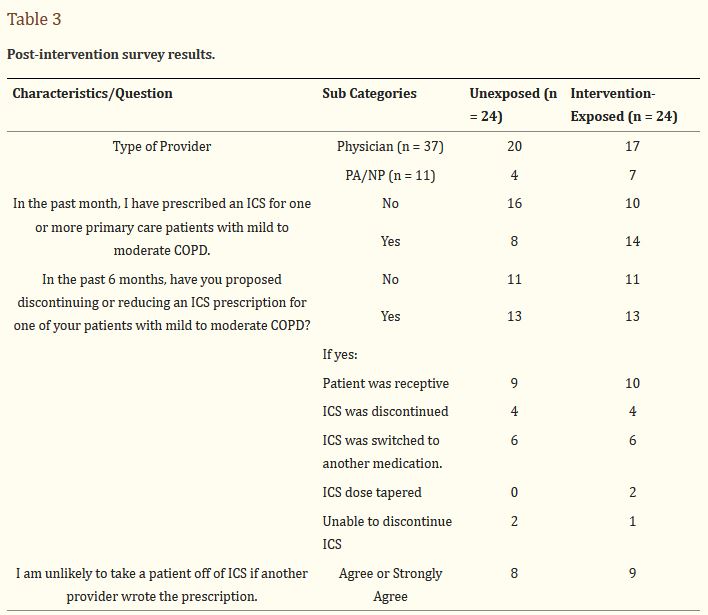
The researchers conducted a mixed-methods analysis in a provider-randomized quality improvement project which involved proactive electronic consultation from pulmonologists recommending ICS discontinuation when appropriate and included PCPs at two VHA systems.
Interviews were completed with 16 unexposed providers and six intervention-exposed providers. In addition, the authors interviewed nine patients within three months after their PCP proposed ICS discontinuation. Surveys were returned by 48 PCPs—24 exposed and 24 unexposed—for a 35% response rate.
“The unexposed providers anticipated their patients might resist ICS discontinuation because it seems counterintuitive to stop something that is working, patient’s fear of worsening symptoms or if the prescription was initiated by another provider. Intervention-exposed providers reported similar experiences in post-intervention interviews,” the researchers recounted. “Unexposed providers anticipated that patients may accept ICS discontinuation, citing tactical use of patient-centered care strategies.”
They said intervention-exposed providers who had successfully discontinued an ICS made similar points, adding, “Veterans reported acceding to their providers out of trust or deference to their advanced training, even after describing an ICS as a ‘security blanket.’ Our survey findings supported the subthemes from our interviews. Among providers who proposed discontinuation of an ICS, 76% reported that they were able to discontinue it or switch to another more appropriate medication.”
- Growdon ME, Espejo E, Jing B, Boscardin WJ, Zullo AR, Yaffe K, Boockvar KS, Steinman MA. Attitudes toward deprescribing among older adults with dementia in the United States. J Am Geriatr Soc. 2022 Mar 10. doi: 10.1111/jgs.17730. Epub ahead of print. PMID: 35266141.
- Parikh TJ, Stryczek KC, Gillespie C, Sayre GG, Feemster L, Udris E, Majerczyk B, Rinne ST, Wiener RS, Au DH, Helfrich CD. Provider anticipation and experience of patient reaction when deprescribing guideline discordant inhaled corticosteroids. PLoS One. 2020 Sep 17;15(9):e0238511.
