PORTLAND, OR—A thrashing form of sleep behavior is much more common among military veterans who suffer from post-traumatic stress disorder or concussion, compared to the general population.
Now, researchers at the VA Portland Health Care System and Oregon Health & Science University are trying to determine whether REM sleep behavior disorder might be an early warning of neurodegenerative conditions such as Parkinson’s disease.
An article in the journal Sleep pointed out that, normally during REM sleep muscles are effectively paralyzed. In cases of RBD, however, brain control of muscle paralysis is impaired, resulting in patients acting out dreams during REM sleep, sometimes causing injuries to themselves or their partners.1
While the condition is estimated to affect less than 1% of the general population, 9% of the 394 veterans in the study were diagnosed with RBD, jumping to 21% among those with PTSD.
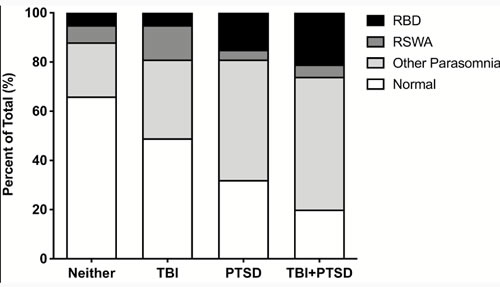
Schematic representation of neuropsychiatric trauma and sleep parasomnia. Subjects with neither a TBI nor PTSD, TBI alone, PTSD alone, and comorbid TBI + PTSD are oriented along the abscissa. For each trauma group, the total percentage of subjects with Normal sleep (clear bar), Other Parasomnia (light fill), RSWA (dark fill), and RBD (totally filled) are shown. Accordingly, the general breakdown between Normal sleep and a parasomnia, within trauma groups, is readily evident. Note the significant percentage of subjects with PTSD or TBI + PTSD that have RBD.
“This is important because, in the general population, RBD has been linked to Parkinson’s disease, and RBD often precedes classic symptoms of Parkinson’s by years,” explained senior author Miranda Lim, MD, PhD, a staff physician at the Portland VAMC and assistant professor of neurology, medicine and behavioral neuroscience in the OHSU School of Medicine. “We don’t know whether veterans who have PTSD and higher rates of RBD will go on to develop Parkinson’s, but it is an important question we need to answer.”
Researchers posited that chronic stress on the brain could play a role in causing the sleep disorder in veterans with PTSD, especially because so many veterans have been exposed to concussion, which potentially accelerates neurodegenerative processes.
For the study, participants underwent an overnight sleep study at the Portland VAMC between 2015 and 2017 to determine the presence of dream enactment during episodes of REM sleep; researchers continuously monitored muscle activity during the eight hours of the study in order to diagnose RBD.
Results indicated that veterans with PTSD had more than a twofold increased odds of RBD compared to those without PTSD.
“RBD seems to be highly prevalent in veterans with a history of trauma,” noted lead author Jonathan Elliott, PhD, a research physiologist at the Portland VA and assistant professor of neurology in the OHSU School of Medicine.
Lim suggested that diagnosing patients with RBD could help identify veterans earlier in the disease course and potentially intervene, adding, “By the time a patient shows classic symptoms of Parkinson’s, it may be too late. If you could intervene when people first start to show RBD, maybe you could prevent later symptoms of Parkinson’s.”
The study team sought to describe the crude prevalence of RBD following traumatic brain injury and PTSD, pointing out the possible relationships between TBI, PTSD, RBD and neurodegeneration.
Participants were 394 mostly male veterans with an average of 54.4; all completed in-lab video-polysomnography and questionnaires. The study team assessed TBI and PTSD using diagnostic screening and medical record review.
The patients were categorized into 4-groups after assessment of REM sleep without atonia (RSWA) and self-reported dream enactment:
- Normal: Neither RSWA nor dream enactment;
- Other Parasomnia: Dream enactment without RSWA;
- RSWA: Isolated-RSWA without dream enactment; and
- RBD: RSWA with dream enactment.
The authors determined that overall prevalence rates were 31%, 7% and 9% for Other Parasomnia, RSWA, and RBD, respectively. They also emphasized that prevalence rate of RBD increased to 15% in PTSD patients [(age adjusted POR: 2.81 (1.17-4.66)] and to 21% in patients with TBI and PTSD [(age adjusted POR: 3.43 (1.20-9.35)].
The study noted that none of the participants met all diagnostic criteria for trauma-associated sleep disorder, and no overt dream enactment was captured on video.
“The prevalence of RBD and related parasomnias is significantly higher in veterans compared to the general population, and are associated with PTSD and TBI+PTSD,” the authors wrote. “Considering the association between idiopathic-RBD and synucleinopathy, it remains unclear whether RBD (and potentially TASD) associated with PTSD or TBI+PTSD similarly increases risk for long-term neurologic sequelae.”
- Elliott JE, Opel RA, Pleshakov D, Rachakonda T, et. Al. Post-traumatic stress disorder increases odds of REM sleep behavior disorder and other parasomnias in Veterans with and without comorbid traumatic brain injury.Sleep, 2019; DOI: 1093/sleep/zsz237f


I am a Physician practicing Integrative Medicine at the VA in Clarksburg WV. I have treated a number of patients who have exhibited symptoms of RBD with good results. Whether these individuals will go on to develop Parkinson’s Disease is as yet unknown and may not be known for another 20-30 years. It may be that left untreated, a metabolically injured brains would continue on a degenerative track. Treatments that have helped our veterans include Osteopathy, Acupuncture, Nutritional supplementation. They are also seen in Wholistic Health for lifestyle counselling. Do the veterans in your study have access to these modalities?