Airway Hyperresponsiveness Increased With Oxidative Distress
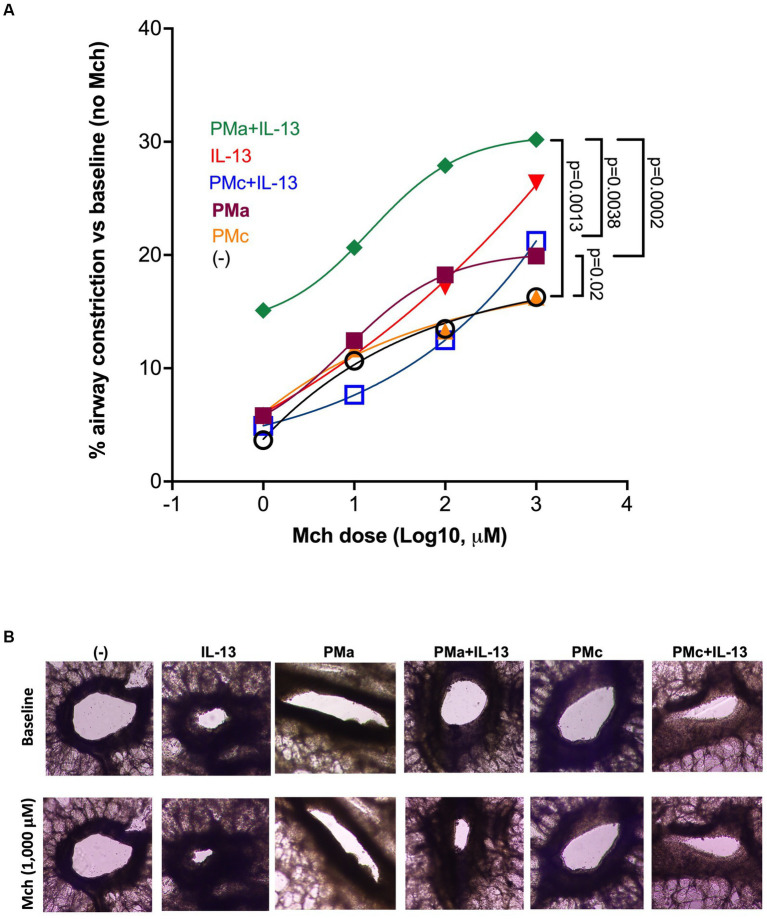
Click to Enlarge: PMa increases airway constriction in human precision-cut lung slices exposed to IL-13. (A) After 72 h, PMa treated PCLS showed an increase in airway constriction and that was significantly increased with the addition of IL-13. Data is represented as a mean from 5 donors. PMa, PM from Afghanistan; PMc, PM from California. (B) Representative images from human precision-cut lung slices showing small airway constriction following methacholine (Mch) challenges under different treatment conditions. The images were taken under a phase contrast microscope at ×10 magnification. Source: Frontiers in Medicine
DENVER — U.S. military personnel who served in Iraq and Afghanistan often present with deployment-related asthma-like symptoms, including distal airway obstruction.
The mechanisms responsible for the development of distal airway obstruction in the deployed exposed to desert particulate matter (PM) are not well understood, according to a report in Frontiers in Medicine.1
A study team from National Jewish Health in Denver sought to determine whether respiratory exposure to PM from Afghanistan (PMa) increases human distal airway hyperresponsiveness (AHR) with or without exposures to IL-13, a type 2 cytokine. The researchers further tested whether mitochondrial dysfunction, such as ATP-signaling and oxidative stress, might be contributing to PMa- mediated AHR.
“This study for the first time demonstrates that PMa exaggerated airway constriction in human distal lungs with high type 2 inflammation,” according to the researchers. “Mechanistically, oxidative stress and mitochondrial dysfunction, such as ATP release and signaling, may contribute to worsened airway obstruction induced by both PMa and IL-13 exposures. Our improved understanding of PM-mediated airway obstruction may provide new insights into mechanisms of deployment-related respiratory disease and potential therapeutic approaches.”
For the study, precision-cut lung slices from donors without a history of lung disease, tobacco smoking or vaping were pre-treated with IL-13 for 24 hours. That was followed by exposure to PMa or PM from California (PMc, control for PMa) for up to 72 hours.
Researchers assessed the role of hydrogen peroxide and ATP in AHR using the antioxidant enzyme catalase or an ATP receptor P2Y13 antagonist MRS2211, also measuring AHR in response to methacholine challenges and cytokine IL-8 production.
The study found that PMa alone, but not PMc alone, was associated with an increase in AHR. “Importantly, the combination of PMa and IL-13 significantly amplified AHR compared to control or PMc+IL-13,” the authors wrote. “PMa alone and in combination with IL-13 increased IL-8 as compared to the control. PMa increased H2O2 and ATP. MRS211 and catalase reduced AHR in PCLS exposed to both PMa and IL-13.”
The researchers said their data suggested that PMa in a type 2 inflammation-high lung increased AHR in part through oxidative stress and ATP-signaling.
The findings are important because nearly 3 million U.S. military personnel have served in Afghanistan and Iraq since 2001, and 14% of those reported deployment-related, asthmalike symptoms, according to the report.
“Environmental hazards from areas of deployment, such as sandstorms, burn bits, and combat dust, are linked to respiratory complications post deployment,” the authors pointed out. “Common respiratory [symptoms] reported include exertional dyspnea, cough, chest tightness, and wheezing.”
The study noted that PM from each of those areas “has a unique composition since there is variable exposure to diesel byproducts, metals, and other toxins. Regardless, parts of their surface composition, such as LPS, can act as Toll-like receptor ligands, which initiate an inflammatory response. Since PM is often coated with metals, PM exposures may lead to production of reactive oxygen species (ROS) and subsequent mitochondrial dysfunction.”
Mitochondrial Dysfunction
Mitochondrial dysfunction stemming from damage or stress is linked to asthma and chronic obstructive pulmonary disease (COPD),” according to the research.
“A key feature of allergic asthma is airway hyperresponsiveness, which is characterized as narrowing of the airway lumen,” the authors added. “The type 2 cytokine IL-13 plays a direct role in the recruitment of eosinophils during allergic inflammation, as well as in epithelial remodeling.”
In another recent study, VA researchers discussed how deployed servicemembers were potentially exposed to high levels of fine particulate matter and other pollutants from a range of sources, including dust storms, burn-pit emissions from open-air waste-burning, local ambient air pollution. In addition, according to the report in Current Opinion in Pulmonary Medicine, they participated in military service-related activities that also could generate airborne exposures.2
Authors from the VA Boston Healthcare System and the San Francisco VAMC reviewed exposures and potential health effects. The goal was to provide a framework for evaluation.
“Particulate matter exposures during deployment exceeded U.S. National Ambient Air Quality Standards,” the researchers wrote. “Epidemiologic studies and case series suggest that, in post-deployment veterans with respiratory symptoms, asthma is the most commonly diagnosed illness.”
They advised that small airway abnormalities, especially constrictive bronchiolitis, have been reported in a small number of deployed, although many haven’t received any established diagnoses for their respiratory symptoms.
The study pointed out that the Promise to Address Comprehensive Toxics Act was enacted to provide care for conditions presumed to be related to deployment exposures, yet “Rigorous study of long-term, post-deployment health has been limited.”
The researchers concluded that veterans’ post-deployment to Southwest Asia and Afghanistan with respiratory symptoms “should undergo an exposure assessment and comprehensive medical evaluation. If required, more advanced diagnostic considerations should be utilized in a setting that can provide multidisciplinary expertise and long-term follow-up.”
- Cervantes D, Schaunaman N, Downey GP, Chu HW, Day BJ. Desert particulate matter from Afghanistan increases airway obstruction in human distal lungs exposed to type 2 cytokine IL-13. Front Med (Lausanne). 2023 Jun 28;10:1177665. doi: 10.3389/fmed.2023.1177665. PMID: 37448802; PMCID: PMC10336202.
- Garshick E, Blanc PD. Military deployment-related respiratory problems: an update. Curr Opin Pulm Med. 2023 Mar 1;29(2):83-89. doi: 10.1097/MCP.0000000000000946. Epub 2023 Jan 4. PMID: 36597757; PMCID: PMC9929891.
