Gulf War Illness Affected One-Third of Veterans of 1991 War
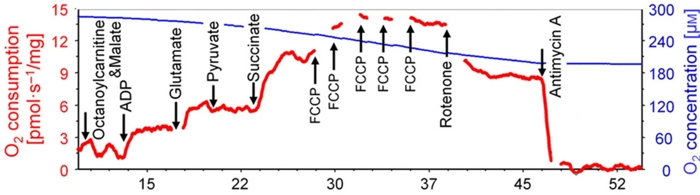
Click to Enlarge: Oroboros methodology figure from the Oroboros website, illustrating addition of different substrates and inhibitors at distinct timepoints. Source: Scientific Reports
SAN DIEGO — Future clinical interventions for Gulf War Illness should focus on impaired mitochondrial function, not inflammation, according to a new study.
Gulf War Illness (GWI) is a chronic, multisymptom health condition affecting one-third of all veterans who served in the 1991 Gulf War. More than 30 years later, most continue to have symptoms, including fatigue, headaches, muscle aches, joint pain, diarrhea, insomnia and cognitive impairment from the condition, which is triggered by veterans’ exposure to environmental toxins.
Debate has continued, however, in the exact mechanism in the body, which has made it difficult to diagnose and treat. Because inflammatory markers are modestly higher in affected veterans than in healthy controls, that has been considered the primary basis of the illness.
In the new study, University of California San Diego School of Medicine researchers assessed information on inflammation vs. mitochondrial function, a rival hypothesis, in 36 individuals, 19 of whom were veterans with GWI. Results were published in the journal Scientific Reports.1
“This is a radical rethinking of the pathology of GWI,” said corresponding author Beatrice Golomb, MD, PhD, professor of medicine at UC San Diego School of Medicine. “For veterans who have long struggled to get effective care, this discovery could be a real game-changer.”
Until now, no study had directly assessed mitochondrial respiratory chain function (MRCF) on muscle biopsy in veterans with GWI. The researchers recruited 42 participants, half veterans with GWI (VGWI), with biopsy material successfully obtained for 36. Levels of mitochondrial respiratory chain function (MRCF) was determined using the muscle biopsies, while the levels of Inflammation were assessed through blood levels of high-sensitivity C-reactive protein (hsCRP), a common marker of peripheral inflammation.
“Impaired MRCF indexed by complex I and II oxidative phosphorylation with glucose as a fuel source (CI&CIIOXPHOS) related significantly or borderline significantly in the predicted direction to 17 of 20 symptoms in the combined sample,” the study team reported. “Lower CI&CIIOXPHOS significantly predicted GWI severity in the combined sample and in VGWI separately, with or without adjustment for hsCRP.”
Mitochondrial Function
The report also noted that “higher-hsCRP (peripheral inflammation) related strongly to lower-MRCF (particularly fatty acid oxidation (FAO) indices) in VGWI, but not in controls. Despite this, whereas greater MRCF-impairment predicted greater GWI symptoms and severity, greater inflammation did not.”
The authors said they were surprised that, adjusted for MRCF, “higher hsCRP significantly predicted lesser symptom severity in VGWI selectively.” They noted that the findings are in line with a hypothesis in which the increased inflammation observed in GWI is driven by FAO-defect-induced mitochondrial apoptosis.
Statistical analyses found that 17 of the 20 most-common GWI symptoms were statistically related to mitochondrial function, compared to one for inflammation.
“Inflammation does appear to be linked to GWI, but our work suggests that it’s actually a side effect of the primary issue, which is impaired cell energy,” Golomb advised.
Mitochondrial dysfunction was found to explain many of the symptoms, according to the report. Two examples were that mitochondrial dysfunction leads to impaired fatty acid oxidation in GWI patients, which could explain the muscle aches and physical fatigue; and that the brain relies mostly on sugar for energy, with GWI cognitive symptoms relating most strongly to impairment in mitochondrial energy production using sugar as a fuel.
The authors suggested that their findings also have possible implications for other health conditions, including different forms of toxin exposure, aging and even heart disease. Because many of those conditions are characterized by increased inflammation but often don’t respond well to anti-inflammatory drugs, the authors argued that mitochondrial impairment might be an underlying cause.
“This is the first time that direct evidence for the mitochondrial hypothesis of GWI has been reported,” said Golomb. “We hope that it will lead to improved treatment plans for the veterans who have long struggled with this mysterious illness.”
- Golomb, B.A., Sanchez Baez, R., Schilling, J.M. et al. Mitochondrial impairment but not peripheral inflammation predicts greater Gulf War illness severity. Sci Rep 13, 10739 (2023). https://doi.org/10.1038/s41598-023-35896-w
