CVD Is the Most Frequent Cause of Death Among RA Patients
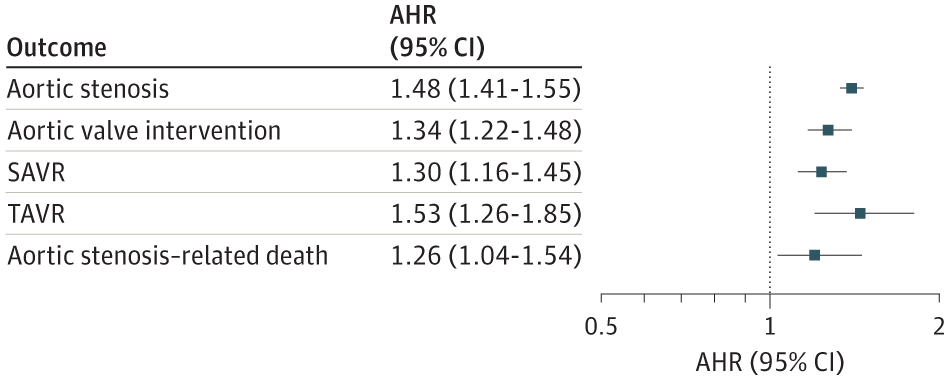
Click to Enlarge: Risk of Aortic Stenosis, Aortic Valve Intervention, and Aortic Stenosis–Related Death in Patients With Rheumatoid ArthritisForest plot illustrates the adjusted hazard ratios (AHRs) and 95% CIs for risk of incident aortic stenosis and aortic stenosis–related outcomes in patients with rheumatoid arthritis compared with matched patients without rheumatoid arthritis. Estimates are from multivariable Cox proportional hazards regression models, stratified on matched pairs and adjusted for race, ethnicity, body mass index, smoking status, comorbidity burden, and health care use. SAVR indicates surgical aortic valve replacement; TAVR, transcatheter aortic valve replacement. Source: JAMA Network
OMAHA, NE — For rheumatoid arthritis patients, cardiovascular disease (CVD) is the most frequent cause of death and leads to much of the excess mortality associated with the condition.
“A substantial body of evidence supports an association between the inflammatory milieu of RA and CVD risk through oxidative stress, endothelial and lipoprotein dysfunction and posttranslational modifications of peptides and subsequent immune responses,” wrote the VA Nebraska-Western Iowa Health Care System-led study.
Less clear is whether rheumatoid arthritis (RA) patients are at increased risk of developing aortic stenosis (AS). In response, the study team conducted a cohort study of 73,070 patients with RA who were matched with 639,268 patients without RA to determine an increased risk of developing AS, undergoing aortic valve intervention and AS-related death.
“Findings of this study suggest that RA is associated with a higher risk of developing AS, as well as the subsequent risks of aortic valve intervention and AS-related death,” the researcher wrote in JAMA Internal Medicine.1
The cohort study linked data from the VHA and the Centers for Medicare & Medicaid Services from 2000 to 2019, matching RA patients by age, sex and VHA enrollment year with up to 10 patients without RA. The researchers followed the cohort until incident AS, aortic valve intervention or death. Data were analyzed from Aug. 23, 2022, to March 3, 2023.
For purposes of the study, aortic stenosis was defined as a composite of inpatient or outpatient diagnoses, surgical or transcatheter aortic valve replacement or AS-related death using diagnostic and procedural codes.
Of the participants with an RA diagnosis, most, 87.6%, were male with a mean age of 63. The matching group had a mean age of 61.9 and 86.7% were males.
With 16,109 composite AS outcomes occurring over 6,223,150 person-years, the AS rate was calculated as 3.97 (95% CI, 3.81-4.13) per 1,000 person-years in patients with RA and 2.45 (95% CI, 2.41-2.49) per 1,000 person-years in the control patients (absolute difference, 1.52 per 1,000 person-years).
The researchers determined that rheumatoid arthritis was associated with an increased risk of composite AS (adjusted hazard ratio [AHR], 1.48; 95% CI, 1.41-1.55), aortic valve intervention (AHR, 1.34; 95% CI, 1.22-1.48), and AS-related death (AHR, 1.26; 95% CI, 1.04-1.54).
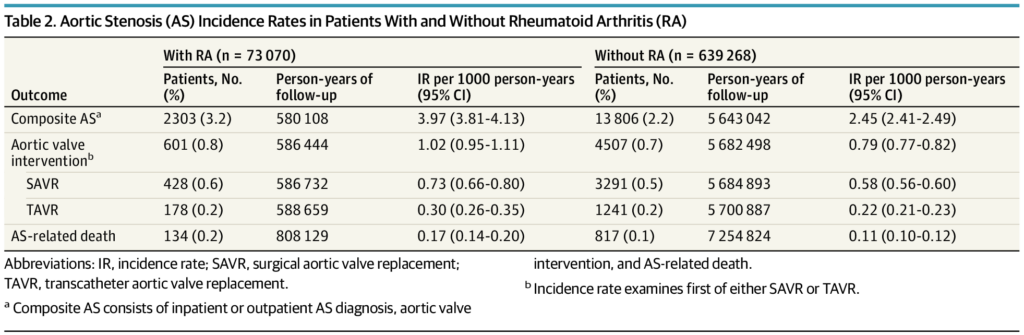
Click to Enlarge: Aortic Stenosis (AS) Incidence Rates in Patients With and Without Rheumatoid Arthritis (RA) Abbreviations: IR, incidence rate; SAVR, surgical aortic valve replacement; TAVR, transcatheter aortic valve replacement.
a. Composite AS consists of inpatient or outpatient AS diagnosis, aortic valve intervention, and AS-related death.
b. Incidence rate examines first of either SAVR or TAVR. Source: JAMA Network
“In this cohort study, RA was associated with a higher risk of developing AS and the subsequent risks of undergoing aortic valve intervention and suffering from AS-related death,” the authors wrote. “Future studies are needed to confirm whether valvular heart disease, specifically AS, may be an overlooked cardiovascular disease complication in RA.”
Background information in the article noted that most studies examining the RA-CVD association have focused on atherosclerotic heart disease and heart failure, but preclinical studies have also revealed the development of valvular carditis in transgenic mice who develop autoantibody-mediated inflammatory arthritis similar to RA. “Additionally, histopathologic analysis of aortic valves in patients without RA and in animal models suggests a pathogenic role of lipoprotein deposition and chronic inflammation in the development of calcific aortic stenosis (AS),” they explained.
The article also pointed out that RA patients have a 75% increased risk of valvular heart disease-related death, which is the most overrepresented cause of CVD death in RA. “However, valvular heart disease is rarely described as an extra-articular manifestation of RA, and investigations in RA have largely been limited to small echocardiographic studies describing the prevalence of valvular abnormalities without longitudinal outcomes,” the researchers advised. “Aortic stenosis is the most common reason for valve replacement and the most frequent cause of valvular heart disease-related death in the U.S. Furthermore, previous case series in RA describe aortitis with adjacent aortic valvulitis and that the aortic valve was the most commonly afflicted valve in previous cross-sectional studies of patients with RA.”
Immune, Inflammatory Mediators
With their findings suggesting that patients with RA had an absolute risk increase of 1.52 composite AS events per 1,000 person-years compared with patients without RA, the authors wrote. “Additionally, patients with RA had a higher risk for aortic valve replacement and AS-related death. These findings support those of preclinical studies depicting the role of immune and inflammatory mediators in the development of valvular carditis. Together, these data support the view that valvular heart disease, specifically AS, may be a CVD complication in RA.”
They added, “After linking with CMS data to capture valvular interventions performed outside the VHA, RA was associated with an increased risk of any aortic valve intervention (AHR, 1.34; 95% CI, 1.22-1.48), including both SAVR (AHR, 1.30; 95% CI, 1.16-1.45) and TAVR (AHR, 1.53; 95% CI, 1.26-1.85), suggesting a more severe AS disease course that required more frequent procedural intervention. This is of particular concern, since patients with RA who underwent SAVR experienced poorer postoperative outcomes in one study.”
The article noted that aggregate inpatient costs per patient undergoing SAVR or TAVR exceeded $60,000 at 6 to 12 months postoperatively.
The researchers reported that RA patients had an increased risk (AHR, 1.26; 95% CI, 1.04-1.54) of AS-related death, which was similar to that of ischemic heart disease in previous RA cohorts. “The findings from the present study emphasize that valvular heart disease may be an underrecognized contributor to the persistent CVD-related mortality gap in RA, particularly given the lack of improvement in AS-specific risk over time,” they emphasized.
In addition to RA-related factors, the study focused on traditional CVD risk factors as risk factors for AS in patients with RA. It found that, consistent with previously reported national health statistics, male sex and hypertension were independently associated with AS onset in RA patients, but other traditional risk factors, including smoking status, diabetes and coronary artery disease, were not.
“In contrast to the so-called obesity paradox in RA in which patients with underweight have a greater risk of CVD mortality compared with patients with overweight or obesity, we found that BMI ≥30 was associated with AS and AS-related death,” the researchers added. “This finding suggests a unique interaction between obesity and AS, potentially through pathways mediated by oxidized lipoproteins. Further study delineating the contribution of metabolic syndrome to AS-related risk in this population is warranted.”
- Johnson TM, Mahabir CA, Yang Y, et al. Aortic Stenosis Risk in Rheumatoid Arthritis. JAMA Intern Med. Published online July 31, 2023. doi:10.1001/jamainternmed.2023.3087

