VA Study: More Depression Patients Should Get Access to Talk Therapy
BOSTON – Nationwide, about a fourth of patients diagnosed with major depression are treated with talk therapy by a trained counselor. Many more might prefer that approach to taking medication, but significant barriers keep access to psychotherapy limited, according to a new study involving VA researchers.
Yet, according to Harvard Medical School, University of Michigan and VA researchers and colleagues, the costs and benefits of the two approaches end up being equal after five years for patients with major depression.
The report in Annals of Internal Medicine suggested that more people newly diagnosed with depression should be given a chance to try individual and group sessions of cognitive behavioral therapy as their first treatment, if that is their preference over antidepressant medication.1
“One might assume that antidepressants are more cost-effective than psychotherapy, because they don’t require travel time, time away from work, and as many contacts with providers as therapy does,” explained first author Eric L. Ross, MD, a psychiatrist at Harvard Medical School, Massachusetts General Hospital, and McLean Hospital. “But when incorporating the long-term effectiveness of each treatment, we found that neither treatment is consistently superior to the other.”
The authors pointed out that most guidelines for major depressive disorder recommend initial treatment with either a second-generation antidepressant or cognitive behavioral therapy and said they wanted to quantify the cost-effectiveness of the two methods of treating an initial diagnosis of depression.
Using a decision analytic model, the study funded by the VA and the NIH sought to determine relative effectiveness from a meta-analysis of randomized controlled trials; additional clinical and economic data from other publications.
Researchers focused on adults with newly diagnosed major depressive disorder in the United States over a one to five year period. Included in outcomes measures were costs in 2014 U.S. dollars, quality-adjusted life-years (QALYs), and incremental cost-effectiveness ratios.
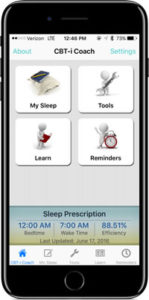
The VA offers the mobile app CBT-i Coach for patients engaged in CBT-I with a health provider, or who have experienced symptoms of insomnia and would like to improve their sleep habits.
In model projections, the authors reported that CBT produced higher QALYs (3 days more at 1 year and 20 days more at 5 years) with higher costs at 1 year (health care sector, $900; societal, $1500) but lower costs at 5 years (health care sector, −$1800; societal, −$2500).
In probabilistic sensitivity analyses, meanwhile, antidepressant treatment had a 64% to 77% likelihood of having an incremental cost-effectiveness ratio of $100 000 or less per QALY at 1 year; CBT had a 73% to 77% likelihood at five years. The relative risk for relapse of depression contributed the most to overall uncertainty in the optimal treatment, according to the researchers.
The authors concluded that neither option “provides consistently superior cost-effectiveness relative to the other. Given many patients’ preference for psychotherapy over pharmacotherapy, increasing patient access to CBT may be warranted.”
“Since CBT and antidepressants are roughly equivalent from a health-economic perspective, other factors should determine what treatment an individual patient receives — and the most important factor is the patient’s values and preferences,” added senior author Kara Zivin, PhD, a professor of psychiatry at the University of Michigan Medical School and a member of the VA Center for Clinical Management Research.
The study noted that, while the majority of people with depression would prefer to receive therapy instead of medications, but only one-quarter of them actually receive therapy. It pointed out that VHA has succeeded in increasing the percentage of veterans receiving CBT in recent years.
“Often we think about these calculations in the short term, because insurance coverage is year to year,” Zivin emphasized. “But if we see effects like these in under five years, perhaps our society will be more willing to bear the upfront costs in order to avoid the indirect costs of missed work and under-productivity later on.”
- Ross EL, Vijan S, Miller EM, Valenstein M, Zivin K. The Cost-Effectiveness of Cognitive Behavioral Therapy Versus Second-Generation Antidepressants for Initial Treatment of Major Depressive Disorder in the United States: A Decision Analytic Model. Ann Intern Med. 2019 Oct 29. doi: 10.7326/M18-1480. [Epub ahead of print] PubMed PMID: 31658472.

