Gastrointestinal Procedures Increase Risks
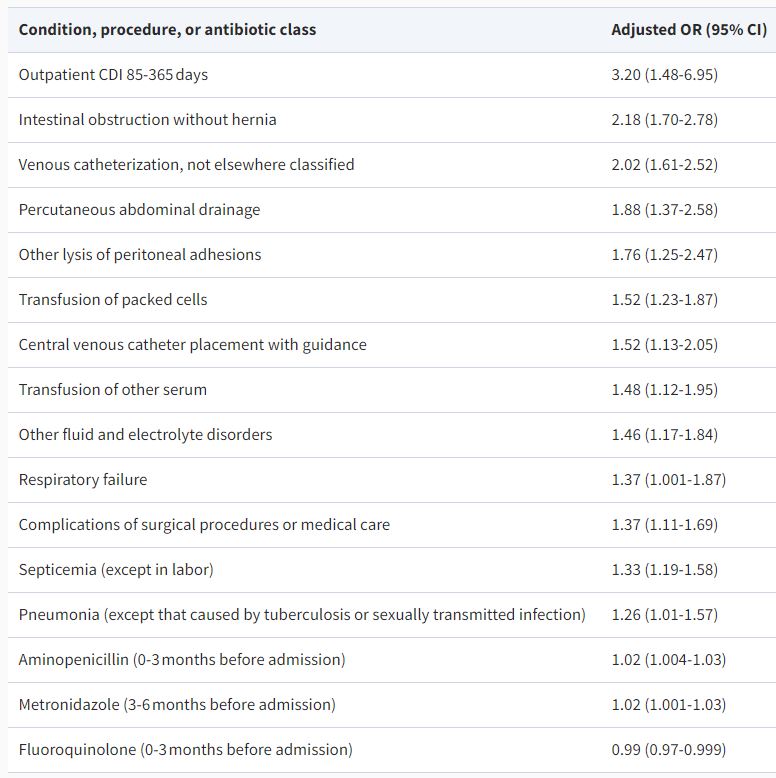
Click to Enlarge: Comorbid Clinical Diagnoses, Procedure Classifications (CCS Codes), and Outpatient Antimicrobial Exposures Most Strongly Associated with HO-CDI – ICD-9 CM codes for diagnoses and procedures were grouped into clinically relevant categories using the Healthcare Cost and Utilization Project’s Clinical Classification Software (CCS). For antibiotic prescriptions, the adjusted odds’ ratio represents the odds of healthcare facility-onset Clostridioides difficile infection (HO-CDI) with each additional day the antibiotic was prescribed during that time period. Source: Military Medicine
BETHESDA, MD – One of the largest studies ever of healthcare-facility-associated Clostridioides difficile infection (CDI) underscored the seriousness of the infection, which causes significantly increased length of stay, higher costs, and, worst of all, greater mortality among inpatients.
The report in Military Medicine called CDI “a rising public health threat.” Uniformed Services University-lead researchers sought to increase understanding of the epidemiology of the infection and also measure the attributable cost, length of stay, and in-hospital mortality within the MHS.
To do that, the study team performed a case–control and cross-sectional inpatient study of hospital-onset (HO-CDI) using MHS database billing records. The focus was on adults admitted to a military treatment facility with a stool sample positive for C. difficile obtained three or more days after admission.
Among 474,518 admissions within the MHS from 2008 to 2015, 591 (0.12%) patients were found to have HO-CDI. Researchers advised that they found a significant increase in the trend of HO-CDI over the 7-year study period.
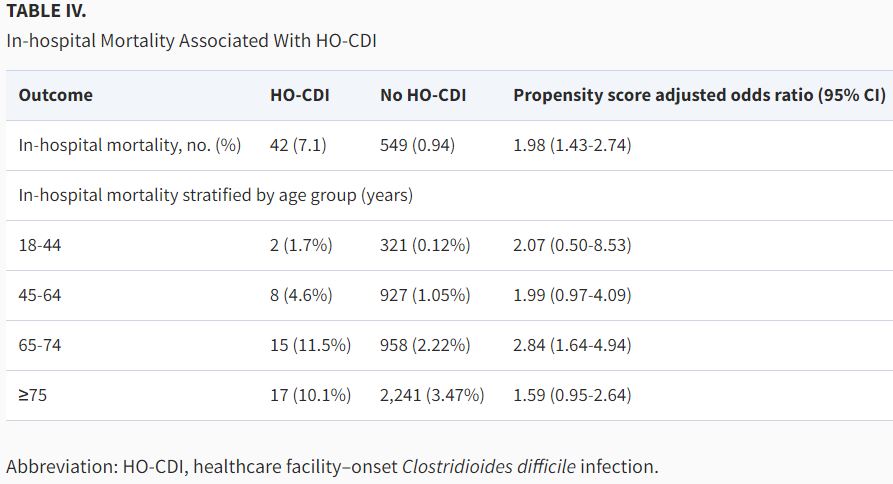
Results indicated that patients with HO-CDI had dramatically higher hospitalization cost (attributable difference $66,044, P < .001), prolonged hospital stays (attributable difference 12.4 days, P < 0.001), and significantly increased odds of in-hospital mortality (case-mix adjusted odds’ ratio 1.98; 95% CI, 1.43-2.74).
“Healthcare facility–onset Clostridioides difficile infection is rising in patients within the MHS and is associated with increased length of stay, hospital costs, and in-hospital mortality,” the authors noted. “We identified a significantly increased burden of hospitalization among patients admitted with HO-CDI, highlighting the importance of infection control and antimicrobial stewardship initiatives aimed at decreasing the spread of this pathogen.”
Background information in the article discussed how the toxin-producing bacterium Clostridioides difficile, which causes watery diarrhea as often as 10 to 15 times a day, “has emerged as a leading healthcare-associated infection and accounts for nearly 500,000 new infections, an estimated 29,000 deaths, and over $4.8 billion in healthcare costs each year in the USA. Less is known about the epidemiology and outcomes of patients with healthcare facility–onset C. difficile infection (HO-CDI), which is defined as laboratory-identified C. difficile infection (CDI) from samples collected more than 3 days after hospital admission.”
Other common symptoms include abdominal cramping and pain, rapid heart rate, dehydration, fever, nausea, increased white blood cell count and kidney failure.
Clostridioides difficile infection in the inpatient setting involves both community and hospital-based transmission, but this study’s focus was on cases acquired in the hospital.
MHS Database
Researchers used the MHS database, which contains laboratory and clinical data on a very large, demographically, and geographically diverse population of patients with universal access to care.
The authors suggested that the reasons for an increasing trend of HO-CDI during the study period were multifactorial:
- higher prevalence of CDI,
- increased testing among hospitalized patients, and
- increased utilization of highly sensitive polymerase chain reaction.
Citing multiple studies finding that advanced age is associated with increased risk of CDI, the authors reported, “Similarly, patients with HO-CDI in our cohort were predominantly older males. Compared to other TRICARE regions, cases of HO-CDI were more often encountered in the TRICARE West region. This may be a reflection of the case-mix and underlying CDI risk factors of patients cared for in these MTFs.”
In addition, the study team said its analysis revealed that certain populations had increased odds of HO-CD because of comorbid conditions and procedures. “Consistent with what is known about C. difficile as a pathogen-causing recurrent infection in up to 35% of patients, our study demonstrated HO-CDI was strongly associated with prior C. difficile infection in the 3-12 months preceding hospitalization, indicating that these patients are prone to repeat infection,” the researchers wrote. “We also found that procedures involving the manipulation of the gastrointestinal tract were associated with increased odds of HO-CDI.”
The study noted that previous research have suggested that patients undergoing gastrointestinal surgery or receiving tube feedings are at higher risk of developing CDI.
Among the other factors, the authors pointed out, was that “healthcare facility–onset Clostridioides difficile infection was also associated with serious bacterial infections such as sepsis and pneumonia, which typically require treatment with broad-spectrum antibiotics and lead to prolonged hospitalizations.”
“The explanation for an association between HO-CDI and procedures such as central venous catheter placement and transfusion of blood products is less clear, but these conditions describe a population of critically ill patients likely hospitalized in the intensive care unit, an environment with multiple known risk factors for C. difficile acquisition and infection, including high colonization pressure and frequent exposure to gastric acid suppressants and broad-spectrum antibiotics,” they added.
On the other hand, this study did not find that outpatient exposure to oral antibiotics such as amoxicillin/clavulanate, third-generation cephalosporins, and clindamycin before hospitalization, had any association with HO-CDI, despite previous research positing a link. “Although our study was unable to track inpatient medication use, it seems plausible that the patients who developed HO-CDI may have received antimicrobials only after admission to the hospital, thus emphasizing the need for judicious use of antibiotics in hospitalized patients. It is estimated that 50% of antibiotic prescriptions in the hospital setting are unnecessary,” according to the article.
As testimony to how serious CDI infection can be, the researchers pointed out that the median length of stay following diagnosis of CDI was 5 days in their cohort, which was comparable to the entire length of stay for the controls. “This supports our assertion that the excess hospital days encountered among HO-CDI patients likely represent a sequela of this infection rather than a cause,” the authors wrote, adding, “Subsequent inpatient admissions with recurrent CDI cost an additional $10,580, with 1.9 days in extended stay compared with primary infection. Overall, our study of HO-CDI demonstrated much longer hospital stays, higher costs, and higher attributable mortality rates associated with this infection, revealing a greater hospital burden of HO-CDI than previously described.”
Calling for future research on how to mitigate hospital spread of the pathogen, the researchers said their findings “confirm the serious nature of this infection and considerable burden it places on healthcare resources.”
- Eberly MD, Susi A, Adams DJ, Love CS, Nylund CM. Epidemiology and Outcomes of Patients With Healthcare Facility-Onset Clostridioides difficile Infection. Mil Med. 2022 Jul 1;187(7-8):e915-e920. doi: 10.1093/milmed/usab116. PMID: 33772561.