Click to Enlarge: Trend of Levothyroxine Use Between 2008 and 2018 by Thyroid Function Categories T4 indicates thyroxine. Source: JAMA Internal Medicine
ANN ARBOR, MI — Clinicians can find it difficult to manage hypothyroidism in older veterans, who tend to have a greater likelihood of adverse effects because of comorbidities, polypharmacy or both.
A new study discussed the complexities and who is most likely to be put at risk.
The report in the Journal of the Endocrine Society pointed out that thyroid hormone prescriptions have become increasingly common, with levothyroxine, which is used to treat hypothyroidism, now being one of the most frequently prescribed medications in the United States.1
“Population-based studies have shown that older age is a significant predictor for thyroid hormone initiation, with use continuing long-term,” wrote University of Michigan-led authors about their findings, which also were presented at the ENDO 2022 national conference. “Thyroid hormone management in older adults is complicated by the presence of comorbidities and polypharmacy, particularly due to medications that can interfere with thyroid function tests.” Yet, they add, little research has been done on the prevalence of concurrent use of thyroid hormone and interfering medications in older adults.
To remedy that—and to quantify patient characteristics associated with this practice—the research team conducted a population-based, retrospective cohort study of 538,137 thyroid hormone users 65 and older from the Corporate Data Warehouse of the Veterans Health Administration (2004-2017).
“First, we described the prevalence of concurrent use of thyroid hormone and medications that commonly interfere with thyroid function tests (i.e., prednisone, prednisolone, carbamazepine, phenytoin, phenobarbital, amiodarone, lithium, interferon-alpha, tamoxifen),” according to the study. “Then, we performed a multivariable logistic regression analysis to determine patient characteristics associated with concurrent use of thyroid hormone and at least one interfering medication during the study period.”
Included in the model were patient age, sex, race, ethnicity and number of comorbidities information.
Results indicate that 170,261 patients, 31.6%, were on at least one interfering medication while on thyroid hormone during the study period, which had a median follow-up of 56 months. More likely to be associated with concurrent use of thyroid hormone and interfering medications were patients of:
- non-white race [odds ratio (OR) 1.18, 95% confidence interval (CI) 1.15-1.21], compared to white race
- Hispanic ethnicity (OR 1.11, 95% CI 1.08-1.14, compared to non-Hispanic),
- female sex (OR 1.12, 95% CI 1.08-1.15, compared to male sex), and
- those diagnosed with comorbidities (e.g., Charlson-Deyo Comorbidity Score ≥2, OR 2.47, 95% CI 2.43-2.52, compared to zero).
On the other hand, patients 85 and older (OR 0.47, 95% CI 0.46 – 0.48, compared to age 65-74 years) were less likely to be associated with concurrent use of thyroid hormone and interfering medications, researchers note.
Thyroid Function Tests
“Almost one-third of older adults on thyroid hormone were taking medications that have been known to interfere with thyroid function tests,” the authors conclude. “Our study highlights the complexity of managing thyroid hormone replacement in older patients, many of whom are at risk for adverse effects in the context of polypharmacy and comorbidities.”
A study last year quantified the dramatic increase in levothyroxine use in the United States.
Led by researchers from the Mayo Clinic in Rochester, MN, the study had participation from the Central Arkansas Veterans Healthcare System in Little Rock, AR, as well as other academic institutions.
“Levothyroxine is one of the most commonly prescribed drugs in the US, with approximately 7% of the population estimated to have an active prescription,” the authors pointed out in JAMA Internal Medicine. “For non-pregnant adults with subclinical hypothyroidism (thyrotropin level elevated but ≤10 mIU/L and normal free thyroxine [FT4] levels), evidence consistently demonstrates no clinically relevant benefits of levothyroxine replacement for quality of life or thyroid-related symptoms.”
Researchers sought to better understand the use of levothyroxine in the United States over time, analyzing national data for commercially insured and Medicare Advantage enrollees. The retrospective analysis used disidentified administrative claims information linked with laboratory results from OptumLabs Data Warehouse, which includes commercially insured and Medicare Advantage enrollees throughout the United Sates.
Included in the cohort were 110, 842 adults with newly filled levothyroxine prescriptions between Jan. 1, 2008, and Dec. 31, 2018, and who had a thyrotropin level measured within 3 months prior to levothyroxine initiation.
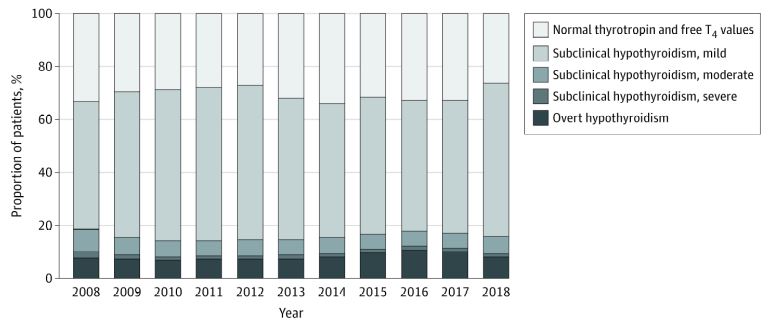
Results indicate that the median thyrotropin level at treatment initiation did not significantly change: 5.8 mIU/L in 2008 to 5.3 mIU/L in 2018 (P = .79). Researchers note that, in a subset of 58,706 patients with thyrotropin and FT4 or T4 levels available, levothyroxine was initiated for overt hypothyroidism (4948 [8.4%]), subclinical hypothyroidism (35 814 [61.0%]), and normal thyroid levels (17 944 [30.5%]).
“From 2008 to 2018, the proportion of adults with overt hypothyroidism increased (7.6% to 8.4%; P = 0.02); the proportion with subclinical hypothyroidism did not change (59.3% to 65.7%; P = 0.36); and the proportion with normal thyroid function did not change (32.9% to 26.2%; P = 0.84),” researchers pointed out. “Among patients with subclinical hypothyroidism, the proportion with mild subclinical hypothyroidism (48.2% to 57.9%; P = 0.73) and moderate subclinical hypothyroidism (8.5% to 6.4%; P = 0.16) did not change significantly, and the proportion with severe subclinical hypothyroidism decreased (2.5% to 1.3%; P = 0.02)”
The study determined that levothyroxine treatment often was initiated for mildly increased thyrotropin levels, which did not vary much over time. In the subset with full thyroid function test results, “60% initiated levothyroxine for treatment of subclinical hypothyroidism (mostly for mild subclinical hypothyroidism) and 30% for normal thyroid function, without significant change in these patterns over time.”
The authors emphasized, “Frequent initiation of levothyroxine in these patients is at odds with evidence demonstrating no significant association of levothyroxine replacement with measures of health-related quality of life, thyroid-related symptoms, depressive symptoms, fatigue, or cognitive function,” concluding that their results “suggest substantial overuse of levothyroxine during the entire duration of the study, suggesting opportunities to improve care.”
- Beeson R, Coe AB, Reyes-Gastelum DR, Haymart MR, Papleontiou M. Interfering Medications in Older Adults on Thyroid Hormone Replacement: Who Is at Risk? Journal of the Endocrine Society, Volume 5, Issue Supplement_1, April-May 2021, Page A831, https://doi.org/10.1210/jendso/bvab048.1694
- Brito JP, Ross JS, El Kawkgi OM, Maraka S, Deng Y, Shah ND, Lipska KJ. Levothyroxine Use in the United States, 2008-2018. JAMA Intern Med. 2021 Oct 1;181(10):1402-1405. doi: 10.1001/jamainternmed.2021.2686. PMID: 34152370; PMCID: PMC8218227.

