Have Fewer Complications Than Those in Outside Care
MENLO PARK, CA— Thanks to the MISSION Act, VA is increasing purchasing healthcare for veterans in the communities where they live.
Proponents of moving more care outside the VA healthcare system suggest that the act improves patient care. While that might be true if patients have difficulty accessing VA services, growing evidence suggests their care generally is as good or better inside the VHA.
A new study in Health Affairs suggested veterans receiving knee replacement surgery at VA facilities generally have fewer complications than those who receive VA-purchased surgery in the community.1
Researchers from the VA Palo Alto Health Care System’s Center for Innovation to Implementation in Menlo Park and colleagues compared post-surgery complications between the two groups. Overall, they found that complication rates were significantly lower for VA-performed surgeries.
Exceptions were found, however, in five locations where VA-purchased care outperformed VA-delivered care. Lead author Alex Sox-Harris, PhD, MS, said in a VA press release that the findings at those sites should not be “misinterpreted to mean those five facilities provided suboptimal care. We did not look at that directly. What we can say is that those five facilities managed to purchase care of even better quality than they delivered.”
The study noted that, “policymakers, administrators, health care providers, and veterans frequently face decisions about which services should be delivered versus purchased by the VA. Comparisons of quality across settings are essential if veterans are to receive care that is consistently accessible, patient centered, effective, and safe.”
The authors suggested that their results provided a path forward for improving orthopedic surgery for veterans, explaining, “As the amount of VA-purchased care continues to increase under the Veterans Access, Choice, and Accountability Act of 2014 and the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act of 2018, these results support VA monitoring of overall and local comparative hospital performance to improve the quality of the care that the VA delivers while ensuring optimal outcomes in VA-purchased care.”
A possible reason for improved outcomes at VA facilities is the focus on assessing pre-operative risk in cohort with a high rate of comorbidities. Other researchers from the Palo Alto Veterans Hospital and Stanford University pointed out that quantifying pre-operative risk is critical to successful surgery, especially those like total knee arthroplasty (TKA) which is resource-intensive and scheduled.
“Studies have demonstrated a wide variety of risk factors, including comorbid conditions, pain, and mental health status, associated with poor outcomes after TKA,” the authors wrote in their report in JB JS Open Access. “As a result, there have been efforts to design preoperative risk assessment tools to help surgeons to risk-stratify and counsel patients3. Unfortunately, currently available surgical risk assessment tools are often cumbersome, requiring patients or providers to manually input various data elements; have limited accuracy; and are poorly adopted. Thus, there remains a need for a preoperative risk assessment tool that is both accurate and efficient for providers.”2
Surgical Risk
On the other hand, researchers pointed out that the VA’s Care Assessment Need (CAN) score, an existing tool developed for primary care providers, uses electronic health record data to automatically calculates risk for individual patients. They posited that the model could present an efficient preoperative risk assessment tool and sought to determine, if the CAN score could be repurposed as a preoperative risk assessment tool for patients proposed for TKA.
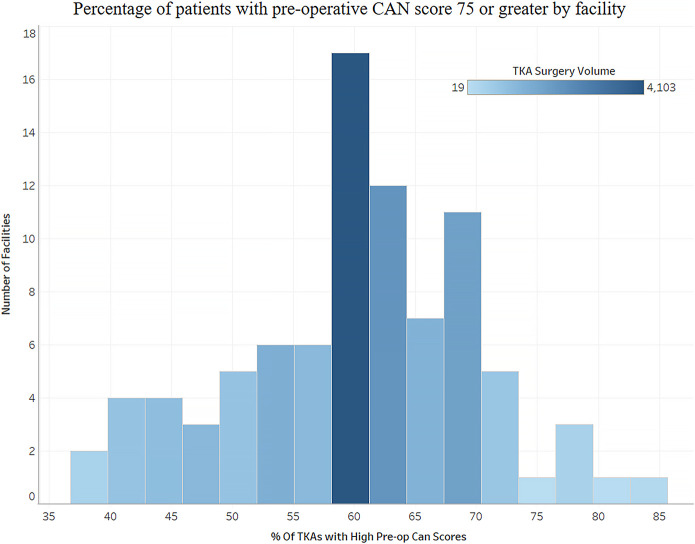
The multicenter retrospective observational study was conducted using national VA data from 2013 to 2016 and included 17,210 veterans who underwent TKA and had a median preoperative CAN score of 75, although there was substantial variability in patient CAN scores among different facilities. The preoperative patient CAN score is a single numerical value ranging from 0 to 99, with a higher score representing greater risk, that is automatically calculated each week using multiple data points in the VA electronic health record.
Listed as the study outcomes of interest were 90-day readmission, prolonged hospital stay (>5 days), 1-year mortality and nonroutine patient discharge.
Researchers found that a preoperative CAN score of greater than 75 was significantly associated with mortality (odds ratio [OR] = 3.54), prolonged length of stay (OR = 1.97), 90-day readmission (OR = 1.65), and nonroutine discharge (OR = 1.57). “The CAN score had good accuracy with a receiver operating characteristic (ROC) curve value of >0.7 for all outcomes except 90-day readmission,” they advised.
Overall, the authors suggested that the CAN score can be leveraged as an extremely efficient way to risk-stratify patients before TKA, with results that surpass other commonly available and labor-intensive alternatives. As a result, this simple and efficient solution is well-positioned for broad adoption as a standardized decision support tool.”
- Harris AHS, Beilstein-Wedel EE, Rosen AK, Shwartz M, Wagner TH, Vanneman ME, Giori NJ. Comparing Complication Rates After Elective Total Knee Arthroplasty Delivered Or Purchased By The VA. Health Aff (Millwood). 2021 Aug;40(8):1312-1320. doi: 10.1377/hlthaff.2020.01679. PMID: 34339235.
- Osborne TF, Suarez P, Edwards D, Hernandez-Boussard T, Curtin C. Patient Electronic Health Records Score for Preoperative Risk Assessment Before Total Knee Arthroplasty. JB JS Open Access. 2020 May 6;5(2):e0061. doi: 10.2106/JBJS.OA.19.00061. PMID: 33123663; PMCID: PMC7418912.