Distant Disease More Common in Younger Patients
SAN DIEGO — The VA treats about 3% of all cases of colorectal cancer (CRC) in the United States each year—6% among cases in men. So, any epidemiological changes have an outsized effect on the nation’s largest integrated healthcare system.
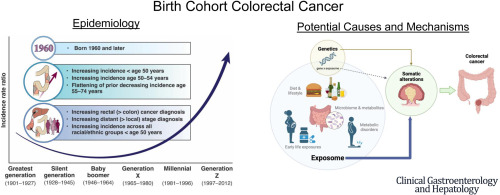
Researchers from VA healthcare systems in San Diego and Los Angeles with related academic medical centers, recently published a review on how dramatically CRC epidemiology is changing due to a birth-cohort effect, including a substantially higher rate of advanced cancer. The trend was first recognized in the last two decades by an alarming increase in early onset CRC (EOCRC) among patients younger than 50.
“In this paper, we define ‘birth cohort CRC’ as the observed phenomenon, among individuals born 1960 and later, of increasing CRC risk across successive birth cohorts, rising EOCRC incidence, increasing incidence among individuals aged 50 to 54 years, and flattening of prior decreasing incidence among individuals aged 55 to 74 years,” the researchers wrote in Clinical Gastroenterology & Hepatology. “We demonstrate birth cohort CRC is associated with unique features, including increasing rectal cancer (greater than colon) and distant (greater than local) stage CRC diagnosis, and increasing EOCRC across all racial/ethnic groups.”
The review pointed out that CRC rates have increased in the United States among individuals born since the early 1960s, adding that Generation X (approximate birth years 1965-1980) experienced an initial increase in EOCRC, and rates subsequently increased among this generation after age 50.
“Compared with individuals born in 1950 to 1954, rates are 1.22-fold (95% confidence interval [CI], 1.15-1.29) higher among individuals born in 1965 to 1969 and 1.58-fold (95% CI, 1.43-1.75) higher among individuals born in 1975 to 1979,” the authors advised. “Rates are now increasing across successive generations, particularly among Millennials (approximate birth years 1981-1996) entering mid-adulthood. Specifically, incidence rates are 1.89-fold (95% CI, 1.65–2.51) and 2.98-fold (95% CI, 2.29-3.87) higher among individuals born in 1980 to 1984 and 1990 to 1994, respectively, compared with individuals born in 1950 to 1954.”
The birth cohort effects have been identified on a global scale, even though population age structure, screening programs, and diagnostic strategies differ across world regions.
“Because birth cohorts age and move through life together, it is anticipated that rates of CRC will continue to increase as time goes on and higher-risk birth cohorts become older,” according to the authors in explaining the implications for the VHA and other healthcare systems.
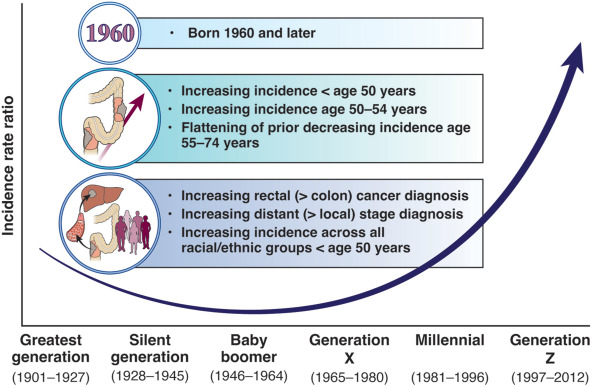
Click to Enlarge: Birth cohort CRC. Birth cohort CRC is defined as the observed phenomenon, among individuals born in 1960 and later, of increasing CRC risk across successive birth cohorts, rising early onset CRC incidence, increasing incidence among individuals aged 50 to 54 years, and flattening of prior decreasing incidence among individuals aged 55 to 74 years. Birth cohort CRC is associated with unique features, including increasing rectal (> than colon) cancer and distant (> local) stage CRC diagnosis, and increasing early onset CRC across all racial/ethnic groups. Source: Clinical Gastroenterology and Hepatology
They explained that four important shifts in CRC incidence are already apparent:
- rates are increasing or plateauing through age 60 to 69 years;
- rectal cancers now predominate through age 50 to 59 years;
- rates of distant-stage disease have more rapidly increased or more slowly decreased compared with local-stage disease; and
- rates of EOCRC are increasing across all racial/ethnic groups.
“These shifts have resulted in changes in the distribution of age and race/ethnicity among individuals diagnosed with CRC over time, with a higher proportion of individuals younger than age 60 years and non-Hispanic Black, non-Hispanic Asian or Pacific Islander (API), non-Hispanic American Indian/Alaska Native (AI/AN), and Hispanic individuals in 2019 vs. 1992,” the researchers explained.
On the other hand, large decreases in incidence rates for age 60-69 and 70-79 years were recognized, although those trends decreased more slowly starting in about 2012. “For example, rates decreased by about 5% per year from 2008 to 2011 for age 60 to 69 years but have since decreased by less than 2% per year,” according to the report. “Similarly, for age 70 to 79 years, rates decreased by almost 6% per year from 2008 to 2013, but by 3.6% per year from 2013 to 2019. Confluence of increasing rates for individuals younger than age 50 years and slowing declines for individuals older than age 60 years has led to stagnating rates for age 50 to 59 years, despite corresponding advances in CRC treatment and declines in risk factors such as smoking.”
The increase in distant stage CRC, suggesting metastasis, has been especially concerning since 1992, the authors advised. “For age 50 to 59 years, local (2008-2019: APC, -0.8; 95% CI, -1.6 to -0.1) and regional (1992-2012: APC, -1.0; 95% CI, -1.4 to -0.6) stage CRC have decreased over time, but distant stage rates (APC, 0.1; 95% CI, -0.1 to 0.3) have remained stagnant (Figure 3C). Distant stage rates have increased most rapidly for ages 30-39 (APC, 3.2; 95% CI, 2.7-3.7) and 40-49 (APC, 2.5; 95% CI, 2.2-2.8) years.
“For age 60 to 69 years, there have been slower declines in distant stage disease (1992-2019: APC, -1.9; 95% CI, -2.1 to -1.6) compared with local (2003-2019: APC, -3.9; 95% CI, -4.4 to -3.5) and regional (2000-2010: APC, -4.7; 95% CI, -5.9 to -3.5) stage, although regional stage rates have slowed in this age group since 2010 (APC, -1.8; 95% CI, -3.0 to -0.6).”
Distant stage rates began to decrease more slowly for age 70 to 79 years (APC, -3.1; 95% CI, -3.4 to -2.8) after 2002, according to the authors, who explained, “Changes in rates by stage could be due to emergence of more aggressive CRC biology but may also be explained by improvements in staging such as imaging.”
The decrease in rates for non-Hispanic whites ages 60-69 and 70-79 years, which make up a large portion of veterans treated by the VA, has been slower than decreases in other racial and ethnic groups. Still, across all age groups, the proportion of patients diagnosed with CRC under age 60, and who are nonwhite has been notable with its increase.
“Taken together, the combined impact of age-related increases in CRC and birth cohort-related trends are likely to result in substantial and important increases in the absolute number of people diagnosed with CRC, particularly among Generation X members now aging into their 50s and 60s,” the researchers wrote.
EOCRC Risk Factors
Another recent VA study suggested that identifying risk factors for early-onset colorectal cancer (EOCRC) could help reverse its rising incidence. Researchers from Richard L. Roudebush VAMC, the Indiana University School of Medicine and the Regenstrief Institute, all in Indianapolis, sought to identify EOCRC risk factors that could be used for decisions about early screening.2
Among 600 cases of sporadic EOCRC [mean (SD) age 45.2 (3.5) years; 66% white], 1,200 primary care clinic controls [43.4 (4.2) years; 68% white] and 1,200 colonoscopy controls [44.7 (3.8) years; 63% shite], independent risk factors were found to include age, cohabitation and employment status, body mass index (BMI), comorbidity, colorectal cancer or other visceral cancer in a first- or second-degree relative (FDR or SDR), alcohol use, exercise, hyperlipidemia, use of statins, NSAIDs and multivitamins. The results were published in Cancer Prevention Research.
In 2021, VA modified its official guidance to recommend that average-risk CRC screening begin at age 45 (down from age 50) in response to the increased incidence of CRC in younger adults.
“The number of CRC cases diagnosed below age 50 among veterans enrolled in VA healthcare has remained relatively stable over the most recent 13 years for which data is available (2010-2022), while the percentage of cases diagnosed below age 50 has increased from about 3% to 6% during that timeframe,” said Michael Kelley, MD, VA’s executive director of national oncology and a professor of medicine at Duke University in Durham, NC. “Further analysis is needed to determine the cause of that increase.”
“For example,” Kelley told U.S. Medicine, “has there been a change in the age of veterans using VA healthcare, or are other factors responsible?”An earlier VA study, which involved 65,940 CRC cases from the National VA Cancer Cube Registry (2001-2015), found that, “while CRC is almost twice as likely to originate from the left colon in the overall population, EOCRC is almost three times as likely to arise from the left side (L:R ratio 2.84). This ratio is highest for cases diagnosed in patients in their 30s (L:R of 3.44).” Those results were published in Cancer Medicine.3
Authors from the Stratton VAMC in Albany, NY, pointed out that left-sided colorectal cancer (LCC) is associated with better survival, compared with right-sided colon cancer (RCC) in metastatic disease. Past studies have indicated that older patients with stage IV left-sided colorectal responded better to treatment and had improved overall survival. The authors questioned whether that was true for patients younger than 50 who have early onset colorectal cancer. The study found that LCC is associated with better OS than RCC only in stage IV for the younger patients compared to the overall population, where LCC is associated with better OS in all stages except stage II. “The better prognosis of stage II RCC might be due to the high incidence of mismatch repair deficient tumors in this subpopulation,” the report advised.
“A consensus is emerging that EOCRC is a pathologically, epidemiologically, anatomically, and biologically different disease than late-onset CRC,” the researchers suggested.
The database included 2,096 EOCRC cases, defined as CRC diagnosed at younger than 50 years old. Results indicated that EOCRC is far more likely to originate from the left side (66.65% LCC in EOCRC vs. 58.77% in CRC). “Overall, LCC has better 5-year Overall Survival (OS) than RCC in stages I (61.67% vs. 58.01%) and III (46.1% vs. 42.1%) and better 1-year OS in stage IV (57.79% vs. 49.49%),” the researchers reported. “Stage II RCC has better 5-year OS than LCC (53.39% vs. 49.28%). In EOCRC, there is no statistically significant difference between LCC and RCC in stages I-III. Stage IV EOCRC patients with LCC and RCC have a 1-year OS of 73.23% and 59.84%, respectively.”
Touted as the first review of primary tumor sidedness (PTS) at the VA, the study noted that, while VA patients are primarily white and male, RCC is more likely to arise in women, Blacks, and the elderly. Right-sided colon cancer also tended to present at a more-advanced stage.
All of that has implications for treatment options. The PARADIGM trial showed longer median overall survival (OS) with first-line mFOLFOX6 plus panitumumab (PAN) vs. bevacizumab (BEV) in patients with RAS wild type (WT), which account for 30% to 50% of CRC patients, and left-sided metastatic colorectal cancer (mCRC; 37.9 vs. 34.3 months, respectively; hazard ratio [HR], 0.82; P=0.031) and similar OS in right-sided patients.4
Based on current guideline recommendations related to clinically relevant biomarkers, Japanese researchers reported clinical outcomes in left-sided mCRC pts with microsatellite stable or microsatellite instability low (MSS/MSI-L) and RAS (KRAS/NRAS)/BRAF (V600E) WT from PARADIGM.
“In left-sided mCRC pts with MSS/MSI-L and RAS/BRAF WT, OS tended to be longer with PAN vs. BEV (40.6 [95% CI, 36.3-44.4] vs. 34.8 [95% CI, 31.3-41.2] months, respectively; HR, 0.79 [95% CI, 0.64-0.97]). Although PFS was comparable between PAN (13.6 months [95% CI, 12.6-15.3]) and BEV (12.6 months [95% CI, 11.3-14.1]; HR, 0.95 [95% CI, 0.77-1.17]), RR and R0 resection rates were higher with PAN (RR: 83.2% [95% CI, 78.0-87.6]; R0: 18.8% [95% CI: 14.2-24.1]) compared with BEV (RR: 66.4% [95% CI, 60.0-72.3]; R0: 10.0% [95% CI: 6.5-14.5]). OS was similar or inferior to PAN vs. BEV, regardless of the primary sidedness in pts with MSI-H or RAS/BRAF mutations.
They concluded that their results supported PAN + mFOLFOX6 as a first-line therapy for left-sided pts with MSS/MSI-L and RAS/BRAF WT.
- Gupta S, May FP, Kupfer SS, Murphy CC. Birth Cohort Colorectal Cancer (CRC): Implications for Research and Practice. Clin Gastroenterol Hepatol. 2023 Dec 9:S1542-3565(23)01005-4. doi: 10.1016/j.cgh.2023.11.040. Epub ahead of print. PMID: 38081492.
- Imperiale TF, Myers LJ, Barker BC, Larson J, Stump TE, Daggy JK. Risk Factors for Early-onset Sporadic Colorectal Cancer in Male Veterans. Cancer Prev Res (Phila). 2023 Sep 1;16(9):513-522. doi: 10.1158/1940-6207.CAPR-22-0506. PMID: 37079701.
- Azar I, Al Masalmeh N, Esfandiarifard S, Virk G, Kiwan W, Frank Shields A, Mehdi S, Philip PA. The impact of primary tumor sidedness on survival in early-onset colorectal cancer by stage: A National Veterans Affairs retrospective analysis. Cancer Med. 2021 May;10(9):2987-2995. doi: 10.1002/cam4.3757. Epub 2021 Apr 2. PMID: 33797856; PMCID: PMC8085929.
- Kentaro Yamazaki et al. Efficacy of panitumumab in patients with left-sided disease, MSS/MSI-L, and RAS/BRAF WT: A biomarker study of the phase III PARADIGM trial.. JCO 41, 3508-3508(2023). DOI:10.1200/JCO.2023.41.16_suppl.3508