VA Study Offers Guidance, Decries Limited Treatment Alternatives
DALLAS—At the VA, proton pump inhibitor prescriptions are first-line treatment for veterans who complain of heartburn and other gastrointestinal reflux issues. The real challenge comes, however, in the more than 30% of cases where PPIs don’t provide enough relief.
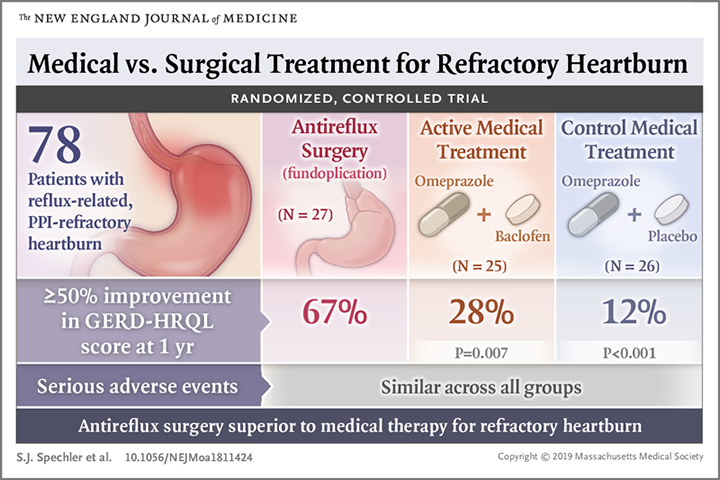
An article in the New England Journal of Medicine discussed a potentially practice-changing study conducted at the VA to provide guidance on when surgery might be the best option.1
“Heartburn that persists despite proton-pump inhibitor (PPI) treatment is a frequent clinical problem with multiple potential causes,” wrote the authors, led by researchers from the VA’s North Texas Healthcare System and Baylor University Medical Center. “Treatments for PPI-refractory heartburn are of unproven efficacy and focus on controlling gastroesophageal reflux with reflux-reducing medication (e.g., baclofen) or anti-reflux surgery or on dampening visceral hypersensitivity with neuromodulators (e.g., desipramine).”
Which treatment is optimal in what cases has far-reaching effect on medical practice, based on the sheer volume of patients with GERD. Background in the article pointed out that, in the United States, about 1-in-5 adults regularly have gastrointestinal reflux symptoms and that annual costs for managing GERD top $12 billion. Yet, that estimate does not take into account loss of work productivity and diminished quality of life in those patients.
Although PPIs are useful for healing reflux esophagitis, according to the report, they tend to be less effective for eliminating GERD symptoms, which persist in about 30% of patients on the drugs.
In fact, only 58% of patients taking prescription PPIs for chronic heartburn report complete satisfaction with their treatment. The result is that “PPI-refractory GERD” is the most common reason for gastroenterologist referrals, according to the report.
To help determine the best approach, the study team focused on 366 patients referred to VA gastroenterology clinics for PPI-refractory heartburn. Those veterans, mean age 48.5 and a majority men, received 20 mg of omeprazole twice daily for two weeks. If heartburn persisted, gastroenterologists then introduced endoscopy, esophageal biopsy, esophageal manometry and multichannel intraluminal impedance-pH monitoring.
“If patients were found to have reflux-related heartburn, we randomly assigned them to receive surgical treatment (laparoscopic Nissen fundoplication), active medical treatment (omeprazole plus baclofen, with desipramine added depending on symptoms), or control medical treatment (omeprazole plus placebo),” the authors wrote. Defined as treatment success in the study was a decrease of 50% or more in the Gastroesophageal Reflux Disease (GERD)-Health Related Quality of Life score (range, 0 to 50, with higher scores indicating worse symptoms) at a year.
Researchers reported that prerandomization procedures excluded 288 patients: 42 had relief of their heartburn during the two-week omeprazole trial, 70 did not complete trial procedures, 54 were excluded for other reasons, 23 had non-GERD esophageal disorders and 99 had functional heartburn (not due to GERD or other histopathologic, motility or structural abnormality).
With the remaining 78 patients undergoing randomization, the study team determined that the incidence of treatment success with surgery (18 of 27 patients, 67%) was “significantly superior” to that with active medical treatment (7 of 25 patients, 28%; P = 0.007) or control medical treatment (3 of 26 patients, 12%; P<0.001).
In fact, researchers pointed out that the difference in the incidence of treatment success between the active medical group and the control medical group was 16 percentage points (95% confidence interval, -5 to 38; P = 0.17).
“Among patients referred to VA gastroenterology clinics for PPI-refractory heartburn, systematic workup revealed truly PPI-refractory and reflux-related heartburn in a minority of patients,” the authors concluded. “For that highly selected subgroup, surgery was superior to medical treatment.”
Continue Reading this Article: Will Surgery Work?

