Few Battlefield Injuries; TRICARE Beneficiaries Opt for Outside Care

The surgery team at Naval Air Station Sigonella in Italy, led by Cmdr. Kennett Moses, orthopedic surgeon, operates on the shoulder of a male patient in September. Members of the 127th Wing Medical Group, and 110th Wing Medical Group, from the Michigan Air National Guard, were training there. Photo by Staff Sgt. Andrew Schumann 127th Wing Public Affairs
BOSTON — Military surgeon readiness continues to decrease because of declining workload, and a new study suggested that patient flow care at the MHS will have to dramatically change to reverse the situation.
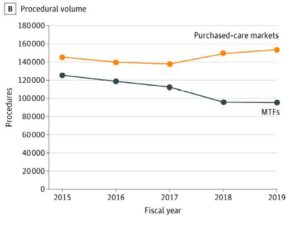
“Changing patterns of care for TRICARE beneficiaries led to a substantial decline between 2015 and 2019 in procedural volume and clinical readiness opportunities for military general surgeons in the MHS, as measured by the novel KSA [Knowledge, Skills, and Abilities] metric,” according to the report in JAMA Surgery. “Already at a low level, the decrease in procedural volume led to a precipitous decrease in the number and percentage of general surgeons reaching the KSA readiness threshold.”1
Harvard Medical School-led researchers added, “Although there have been increases in the number of procedures and KSA points in the purchased-care environment, these increases have not been large enough to fully account for the loss of procedures in MTFs.”
One solution, according to the authors, would be decreasing the use of purchased care, especially in markets that include surgical MTFs.
The cohort study included 147 MTFs facilities and military medical units. It determined that the number of general surgery procedures generating KSAs in military hospitals decreased 25% from fiscal year 2015 to 2019, with a 19% decrease in the number of general surgeons’ KSA points.
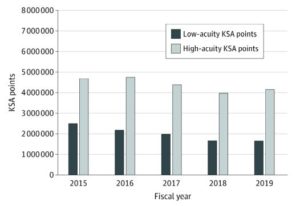
Click to Enlarge: Total General Surgery Knowledge, Skills, and Abilities (KSA) Points Earned in Military Medical Treatment Facilities
Furthermore, according to the study team, “The proportion of military general surgeons meeting the KSA metric readiness threshold decreased from about 17% in 2015 to about 10% in 2019.” In addition to Harvard and Brigham & Women’s Hospital in Boston, researchers were from Rutgers New Jersey Medical School in Newark, the Uniformed Services University of the Health Sciences and Walter Reed National Military Medical Center in Bethesda, MD, as well as Deloitte Consulting in Arlington, VA.
The study pointed out the dual cost of having patients leave MTF-based care for civilian purchased care. One is the hit to clinical readiness. The other is high financial costs associated with the growing use of care purchased in the community outside of military facilities.
“To fulfill the dual-readiness mission of the MHS, institution of policies that lead to increasing the volume of procedures to levels not seen in the past five years may be required, which may necessitate decreasing the use of purchased care, especially in markets that include surgical MTFs,” the study stated. It added that purchased care represents the largest share of DoD healthcare spending and is mounting quickly.
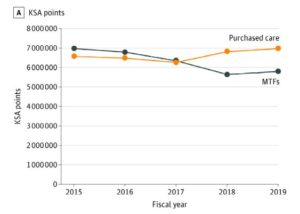
Click to Enlarge: Comparison of General Surgery Knowledge, Skills, and Abilities (KSA) Points and Procedural Volume of Surgical Military Medical Treatment Facilities (MTFs) to Purchased-Care Markets With a Surgical MTFBoth KSA points (A) and procedural volume (B) decreased between 2015 and 2019.
Background information in the article noted that USU, in partnership with the American College of Surgeons, developed the Knowledge, Skills, and Abilities (KSA) Clinical Readiness Program that includes a tool for quantifying the clinical readiness value of surgeon workload. That metric was used to describe changes in U.S. military general surgeon procedural volume and readiness.
Researchers analyzed general surgery workload performed across the MHS, including military and civilian facilities, between fiscal year 2015 and 2019. With data obtained from TRICARE and the DoD health insurance product, the surgeon-level readiness among military general surgeons was calculated based on the KSA metric readiness threshold.
Defined as the chief outcomes of interest were general surgery procedural volumes and the KSA metric point value of those procedures across the MHS, as well as the number of military general surgeons meeting the KSA metric readiness threshold, according to the authors.
Researchers used aggregate facility and regional market-level claims data were used to calculate the procedural volumes and KSA metric readiness value of those procedures. They then calculated annual adjusted KSA metric points earned to determine the number of individual US military general surgeons meeting the readiness threshold.
Results indicated that the number of general surgery procedures generating KSAs in military hospitals decreased from 128 377 in 2015 to 95 461 in 2019, with a decrease in the number of general surgeon KSA points from 7.2 million to 6 million.
In contrast, from 2015 to 2019, there was a 3.2% increase in both the number of procedures –from 419, 980 to 433, 495 –and KSA points — from about 21.1 million to about 22 million in civilian care settings. The percentage of military general surgeons meeting the KSA metric readiness threshold declined from 16.7% (n = 97) in 2015 to 10.1% (n = 68) in 2019, the study advised.
“This study noted that the number of KSA metric points and procedural volume in military hospitals has been decreasing since 2015, whereas both measures have increased in civilian facilities,” the authors wrote. “The findings suggest that loss of surgical workload has resulted in further decreases in military surgeon readiness and may require substantial changes in patient care flow in the MHS to reverse the change.”
Researchers suggested that the KSA metric provides a new way to quantify the readiness value of care. That, they said, will provide better balance with quality metrics and financial costs to improve the MHS.
Optimizing MTF Operations
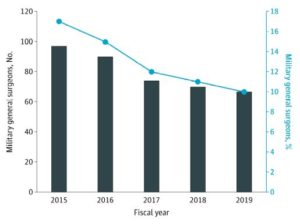
Number and Percent of Military General Surgeons Meeting Knowledge, Skills, and Abilities Readiness Threshold
“There are also opportunities to improve clinical readiness and increase KSA point volumes by optimizing MTF operations,” the authors wrote. “This is of particular importance, given our findings of decreases in total procedural and KSA point volumes in MTFs that are not fully accounted for by increases in purchased care in surgical markets. The readiness mission of the MHS has traditionally focused on providing MTF-based care to active-duty servicemembers, even to the potential detriment of military healthcare professionals’ clinical readiness.”
For example, researchers recommended using KSA point values of procedures “to optimize scheduling for elective operations across specialties and assign priority to cases with more dual-readiness value when operating room capacity is limited. By measuring what matters, the MHS can focus on enhancing its value to provide clinical readiness to combat casualty care medical personnel.”
The study also discussed military-civilian partnerships, which can offer opportunities for military clinicians to practice in civilian medical centers. “In these partnership programs, military surgeons are able to treat a greater volume of patients with high-acuity conditions than are available at most MTFs,” the authors explained.
The study cited successful military-civilian partnerships at some of the busiest trauma centers in the United States and added that the MHS Strategic Partnership at the American College of Surgeons has published a best practices guide for creating and sustaining military-civilian partnerships, The Blue Book.2
Another possibility, according to the authors, would be opening MTF care to non-TRICARE beneficiaries. High-KSA value patient encounters would help improve clinical readiness, and the model is already being used at the trauma centers of Brooke Army Medical Center in San Antonio, TX, and Naval Medical Center Camp Lejeune in Jacksonville, NC, which care for both injured military and civilian patients in their regions.
While TRICARE beneficiaries value the choice of military and civilian hospital settings, the authors emphasized the importance of high-quality patient care and patient experience at military facilities. “Recent work has noted that several MTFs perform in the top tier nationally with respect to surgical quality and safety, and statistical trends toward systemwide improvement have been noted since the implementation of the American College of Surgeons National Surgical Quality Improvement Program in the MHS,” they said.
A commentary on the article pointed out, “A future ideal state likely involves a combination of these and other strategies in which the resources of the military health system are optimally and efficiently used to maintain volumes supporting surgical quality and readiness, while also pursuing complementary recruitment strategies and just-in-time additional training for the deploying surgeon.”
The authors, Lesly A. Dossett, MD, MPH, and Justin B. Dimick, MD, MPH, of Michigan Medicine in Ann Arbor, cautioned, “Without urgent attention to decreasing case volumes for surgeons, the ability to maintain a ready medical force may be threatened.”
Indeed, the article pointed out that declining intensity of fighting in current conflicts has been a factor in reduced experience treating combat casualties. That has raised questions about military surgeon readiness to treat battlefield injuries.
“Throughout modern history, combat casualty care improves during periods of armed conflict only to see these advances diminish in peacetime, a phenomenon known as the peacetime effect or Walker dip,” the authors explained. “To counteract this decline, the US Military Health System (MHS) pursues a dual mission of providing a “medically ready force and ready medical force.” In fulfilment of this mission, care provided in military-owned and -operated hospitals, known as military medical treatment facilities (MTFs), serves not only to promote the health and wellness of service members, but also to ensure the clinical readiness of military health care professionals to provide care in both the MTF and deployed settings.”
While some common surgical procedures, such as vascular and burn surgeries, have clear connections to battlefield injuries, others aren’t as obvious. “The high KSA value of breast surgery, one of the most commonly performed operations in MTFs, is derived from the military surgeon’s need to be able to manage soft-tissue injuries, which are among the most common combat injuries,” researchers wrote. “In addition, abdominal wall and hernia surgery, another higher-volume procedure, has significant combat readiness ties in the management of damage control surgery and eventual abdominal closure.”
- Dalton MK, Remick KN, Mathias M, et al. Analysis of Surgical Volume in Military Medical Treatment Facilities and Clinical Combat Readiness of US Military Surgeons. JAMA Surg. Published online October 27, 2021. doi:10.1001/jamasurg.2021.5331
- The Blue Book: Military-Civilian Partnerships for Trauma Training, Sustainment, and Readiness. American College of Surgeons; 2020.